Burnout is pertinent among healthcare professionals. According to the CDC, nearly half of health workers reported feeling burned out in 2022. That same year, the American Association of Nurse Anesthesiology (AANA) reported that 80% of Certified Registered Nurse Anesthetists (CRNAs) declared high levels of disengagement and exhaustion.
The statistics are a daunting reality and one of the many reasons CRNA work-life balance is of the utmost importance. As a healthcare professional, you deserve to care for yourself as much as you care for your patients.
We’re here to help. Learn how to create your ideal work-life balance with the guidance below.
Table of Contents
- A typical work schedule for CRNAs
- Factors that influence CRNA work-life balance
- 5 tips on maintaining a healthy work-life balance as a CRNA
- How APEX Anesthesia can improve your work-life balance
A typical work schedule for CRNAs
CRNA work schedules are highly variable with some finding employment as part-time or locum tenens. For full-time positions, the schedule often spans 40 to 60 hours per week, typically over four to five days. Additionally, holiday, weekend, and overtime shifts, which can exceed 12 hours, may be required, depending on the employment setting.
When work occupies most of your week, it’s challenging to make time for yourself. Let’s discuss the influential factors impacting CRNA work-life balance below.
Factors that influence CRNA work-life balance

The U.S. Department of Health and Human Services states that excessive workloads, administrative burdens, limited say in scheduling, and lack of organizational support are common causes of health worker burnout. These issues, alongside cultural, financial, and societal pressures, create obstacles when fostering a healthy work-life balance.
Financial stress
Financial stress is burdensome no matter the circumstance. The pressure of working overtime to meet economic needs and the strain of an unmanageable workload typically lead to declining work performance. In fact, 44% of U.S. employees reported personal finance issues as a distraction at work in 2023.
Workload
Work overload is a strong contributing factor to CRNA burnout. A study published in the Journal of General Internal Medicine reported that healthcare workers undergoing work overload had up to 2.9 times the risk of experiencing burnout.
Work location and environment
Long commutes have been associated with poorer mental health and may present a challenge in balancing your professional and personal obligations. A negative workplace environment may also instill stress and unease.
Stress
You’re not alone if you’re experiencing high stress levels at work—work issues account for 49% of stressors among healthcare workers. If you fall into this common category, the AANA provides suggestions for recognizing and managing stress.
5 tips on maintaining a healthy work-life balance as a CRNA

Learn how to avoid CRNA burnout and improve your well-being with the following tips.
Change a factor
We know it’s easier said than done—some factors are simply beyond your control. But you can proactively manage your outlook and maximize existing opportunities. For example, try utilizing long commutes to engage with resources such as audiobooks or podcasts. Implementing small changes helps improve the commuting experience, positively impacting your mental health.
Practice mindfulness
Mindfulness techniques alleviate stress and increase focus. Methods vary by individual preference, but some standard practices are breathing exercises, paying attention to the five senses, and monitoring your internal dialogue.
Quality time with friends and family
Maintaining strong connections with family and friends is highly beneficial for your well-being. Psychological research demonstrates that social connections help individuals lead a long, healthy life and reduce the chances of mental health issues.
Schedule me time
Life as a CRNA should not be exclusively devoted to work. It is highly recommended to allocate time for self-care and participate in activities that alleviate stress, such as exercise. Furthermore, the AANA suggests using time off to combat burnout.
Set healthy boundaries
The desire to be a high-performing CRNA is understandable, but the benefits do not always outweigh the costs. Maintaining clear boundaries between your professional and personal life is essential. Exercise caution when accepting additional responsibilities, as extended work hours often lead to fatigue, which harms your physical health and causes patient safety issues.
How APEX Anesthesia can improve your work-life balance
APEX Anesthesia was created by CRNAs for CRNAs. We understand better than anyone else how busy you are balancing life and work. That’s why we offer CRNA continuing education (CE) online!
Use a desktop or mobile device with APEX to learn anytime, anywhere. Our CE courses are convenient and easy to navigate, helping you earn Class A credits at your own pace and be the most knowledgeable CRNA you can be.
We’ve helped more than 50,000 students and nurse anesthetists. And we can help you, too. Explore our CE bundles and pick the right fit for you.
We knew and greatly admired Dr. John Nagelhout, PhD, CRNA, FAAN, a CRNA whose life of teaching, research, clinical work, and program leadership eclipsed others of his generation. He was revered locally by his students and fellow colleagues and known widely as the principal architect of the book Nurse Anesthesia, the definitive treatise of our specialty. To the tens of thousands who have turned to his text seeking clarity or illumination, the book took on a kind of mythology of its own, referred to by most not by the formal rubric cataloged by the Library of Congress but simply as “Nagelhout.”
John recently passed. He was an elegant, soft-spoken, and humble man whose genius was evident in many ways. Today, we wish to revisit just one of his many accomplishments – our personal way of immortalizing and giving thanks to the man. We must start with the Taiwanese banded krait, a serpent nearly unrivaled for its hellacious venom. This krait’s neurotoxin kills many in its Southeast Asia and Northern China habitats. The primary active ingredient in that venom is α-bungarotoxin (α-Btx), a proteinaceous concoction that binds irreversibly to the nicotinic acetylcholine receptor (nAChr). Like a heat-seeking missile whose sole task is to bore down with savage intensity onto an enemy plane’s heat signature, α-Btx does the same with exquisite biochemical precision as it seeks out the nAChr, blocking the action of ACh. An agonizing paralysis, respiratory failure, and death await the envenomated victim in near-time. John knew this.
 The banded krait (Bungarus fasciatus)
The banded krait (Bungarus fasciatus)
John also knew that skeletal muscle saturated with α-Btx, irreversibly affixes itself to every Ach receptor on a one-to-one basis. Knowing the total amount of α-Btx that is exposed to the skeletal muscle (we will call that ‘α-Btx Total’), and armed with the knowledge that once attached to the nAChr, it stays put (we will call that ‘α-Btx Blocking’), then the amount of free α-Btx recovered (we will call that ‘α-Btx Recovered’) permits the precise quantification of the number of Ach receptors in the muscle sample. That is:
(α-Btx Total) – (α-Btx Blocking) = (α-Btx Recovered)
Now take that little equation a bit further:
(α-Btx Total) – (α-Btx Recovered) = (α-Btx Blocking)
Therefore,
(α-Btx Blocking) = quantification of the amount nAChr
The elegance of the pharmaco-biochemical rationale is foundational to a good deal of past, present, and likely future neuromuscular and neurophysiological research and clinical work. While we’ve simplified the complexities of its measurement, this gives us a good sense of how to determine the density of nAChr in skeletal muscle.
A life-saving observation
As entry-level students in the specialty, we all learned that the administration of succinylcholine to a burn patient (among a few other scenarios as well) could produce nearly instantaneous cardiac arrest due to profound hyperkalemia. Before John’s time, the mechanism was poorly understood, and several hypotheses were proposed, but the science had not kept up.
We contacted a close CRNA colleague and friend of John’s, Valdor Haglund, who worked with him on various clinical and research activities. He shared details about a patient John and other colleagues cared for. The unfortunate man experienced devastating 2nd and 3rd-degree burns over 80-90% of his body and was tended to in the institution’s burn unit for many procedures over a period of many months. John and colleagues designed a study to address their hypothesis, and with full consent, while the patient was under anesthesia for regular burn debridement and grafting procedures, skeletal muscle tissue samples were harvested and exposed to α-Btx. A remarkable observation was made, which lives in infamy and provides a mechanistic explanation that has prevented many deaths, warning us of the perils of using succinylcholine in burn-injured patients. An explanation directly traced back to John.
Here, published with permission, is the original graph from John’s momentous publication in the journal Anesthesiology decades ago. This graph clearly and quantitatively demonstrates the time course of the proliferation of extra-junctional nAChr in a burn patient.
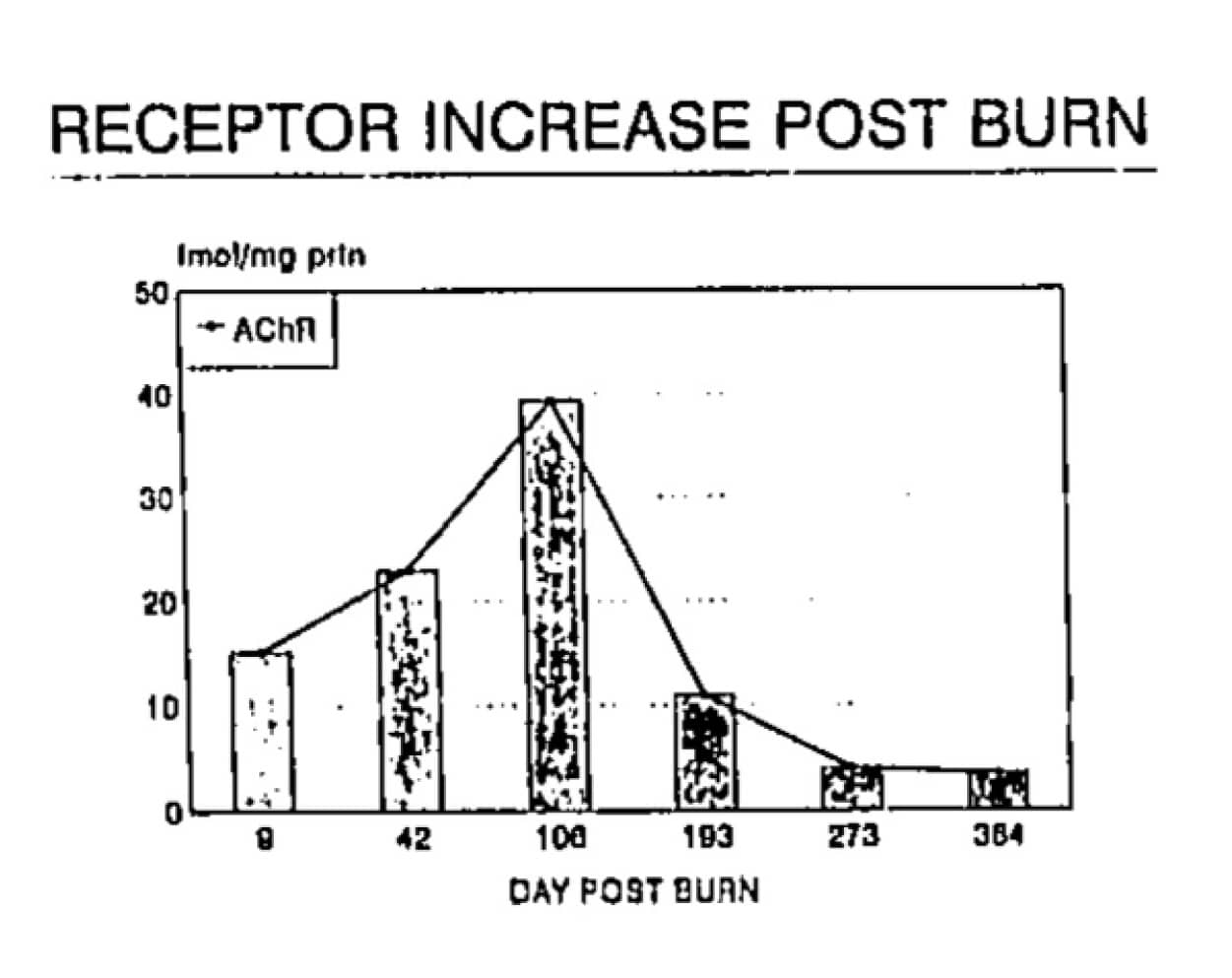
With kind permission. Anesthesiology. September, 1994;81:A1089.
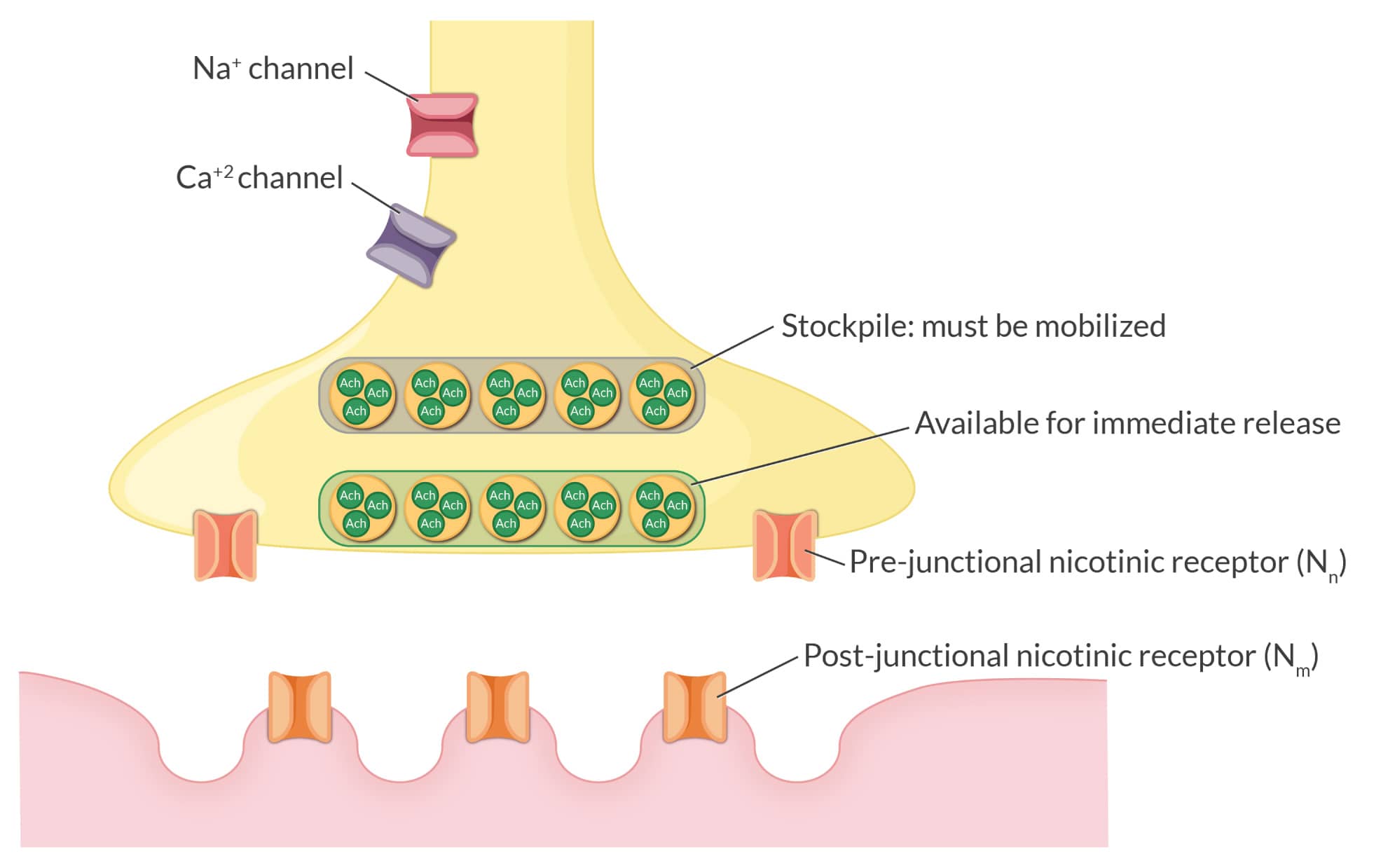
The nAChr in skeletal muscle is usually positioned strategically at the edges of the junctional folds at the neuromuscular junction on the postsynaptic side. Following ACh activation, Na+ and K+ diffusion results in depolarization, permitting muscular contraction in a graded manner. This gradation allows us to precisely quantify skeletal muscle activation, permitting us to lightly brush a baby’s cheek or heave a heavy load of dirt into a wheel barrel. Despite a high intracellular K+ concentration, what is usually liberated into the serum with succinylcholine administration is physiologically insignificant. However, with extrajunctional proliferation of nAChr, creating new “spigots” on the muscle cell membrane for K+ to emerge, serum K+ can rise dramatically and potentially catastrophically. We can look to John for illuminating the precise mechanism for why we must avoid succinylcholine in scenarios of extrajunctional spread of nAChr in burn injury and other scenarios like paralysis, immobilization, and certain myopathies. Thank you, John.
A life that inspired others
John may have been the first CRNA to obtain a PhD in a basic science, who then marshaled that knowledge and skill set to inform the evidence-based practice of anesthesiology using the tools of science guided by a keen intellect. His students and contemporaries lauded him as a polymath, and for good reason. To this day, few can put forth a comparably eclectic and accomplished curriculum vitae of professional and life experience.
Rest in peace, John Nagelhout. We are all grateful for what you accomplished and your legacy of teaching, research, clinical work, and program leadership, which continues to inspire many of us.
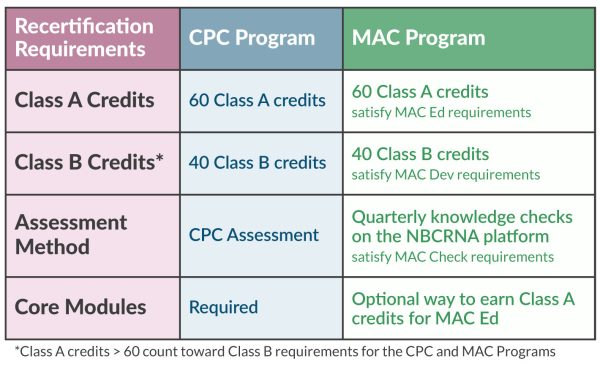
Understanding the requirements for Certified Registered Nurse Anesthetist (CRNA) recertification doesn’t have to be so challenging. Created by the National Board of Certification and Recertification for Nurse Anesthetists (NBCRNA), recertification ensures CRNAs remain at the appropriate skill level to administer safe and proper care.
If you want help understanding the steps to take toward CRNA recertification, you’re not alone. Let us walk you through the requirements!
Table of Contents
- The Maintaining Anesthesia Certification (MAC) Program
- The Continued Professional Certification (CPC) Program
- CPC glossary: What you need to know about the requirements
- How to earn CRNA continuing education credits
The NBCRNA offers two distinct programs to maintain your CRNA certification: the Continued Professional Certification (CPC) Program, and the newly introduced Maintaining Anesthesia Certification (MAC) Program. However, it’s important to note that the CPC Program will be sunsetting on August 1, 2025. After this date, the MAC Program will be the sole pathway for CRNA recertification. We’ll explore both options, so you’ll know exactly what you need to recertify regardless of the program you’re in.
The Maintaining Anesthesia Certification (MAC) Program
NBCRNA recertification requirements have evolved. The new MAC Program will replace the CPC Program, and all CRNAs will be enrolled in the program by 2026.
The MAC Program simplifies the recertification process; it’s a consistent 4-year cycle with the same requirements every cycle!
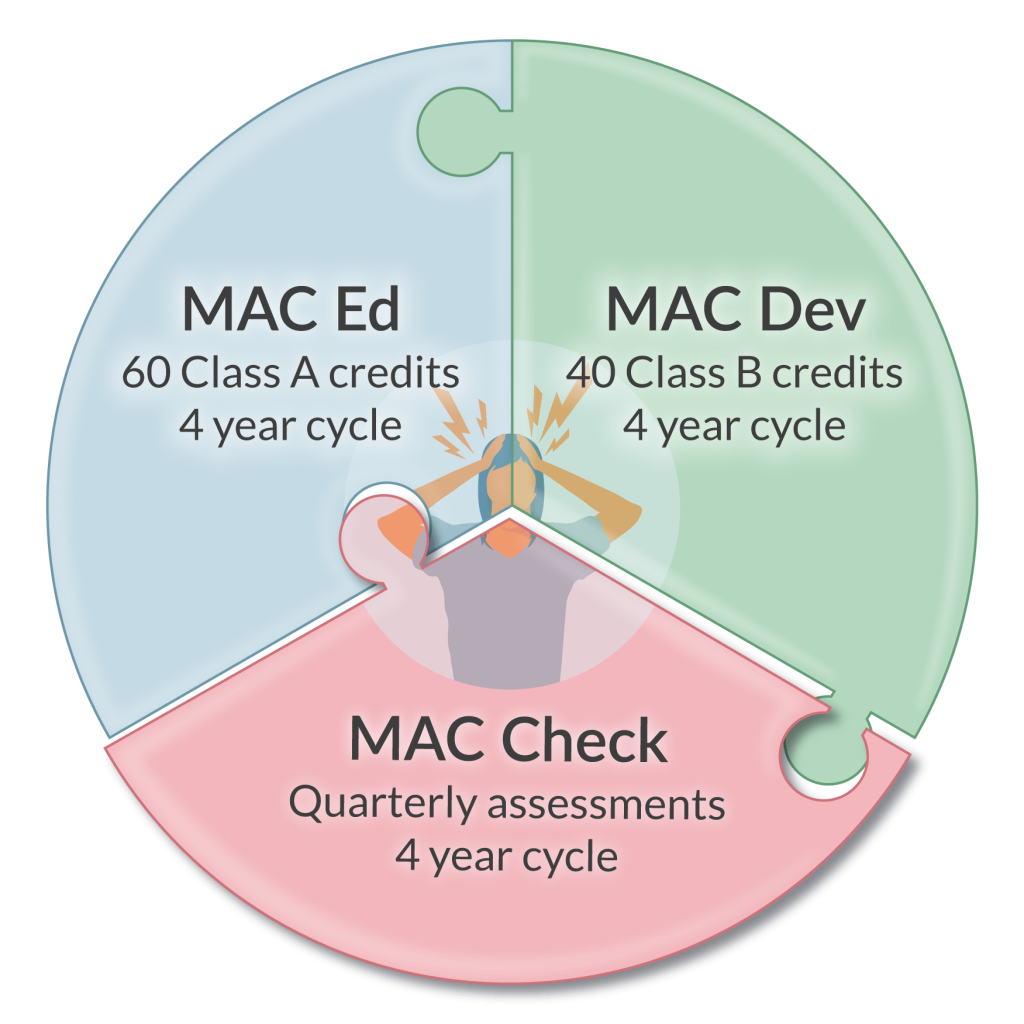
In the MAC Program, you’ll complete:
- MAC Ed (A new name for 60 Class A credits – see details in the Class A Credits section above)
- MAC Dev (A new name for 40 Class B credits – see details in the Class B Credits section above)
- MAC Check (Replaces the CPCA)
Although CPC Core Modules aren’t required for the MAC Program, they’re an efficient way to stay at the forefront of anesthesia practice while earning Class A credits.
What is the MAC Check?
Available on computers and mobile devices, the MAC Check is a longitudinal, quarterly assessment that tracks your progress and performance over a longer period of time.
The MAC Program is divided into 16 quarters. You’ll complete the MAC Check in 13 of the first 15 quarters, and you’ll get to pick 2 quarters where you can skip the MAC Check. Also, you won’t have to complete the MAC Check in your 16th quarter.
How does the MAC Check work?
In your 1st quarter, you’ll complete 25 multiple-choice and multi-select questions. Each question is timed for 1 minute, and you can bank unused time and apply it to subsequent questions. The platform will provide immediate feedback after each question, including the rationale for correct answers. You’ll also be able to view areas for improvement to guide your CE and development activities. In subsequent quarters, you’ll complete up to 30 questions.
If you answer a question incorrectly, you’ll encounter it again in a subsequent quarter. Re-administered questions make up to 5 incorrectly answered questions in each quarter, totaling between 25 to 30 questions.
Once you have completed 4 Mac Check quarters, you’ll receive preliminary feedback to see where you stand in regards to the performance standard. After the 13th knowledge check is completed, you’ll receive a final measurement for that cycle.
Explore the MAC sample to familiarize yourself with the new platform.
What happens if I “fail”?
If you don’t meet the performance standard, you must earn additional 5 MAC Ed (Class A) credits per domain where you don’t meet the passing standard. These credits are in addition to your 60 Class A credit requirement. Like the CPCA, MAC Check is not a pass/fail assessment, and you will not lose your certification so long as you complete the remediation requirements prescribed by the NBCRNA. However, completion of the MAC Check is required.
For more information on credit requirements based on MAC Check performance, please read What Every CRNA Needs to Know about the MAC Program.
The Continued Professional Certification (CPC) Program
The CRNA recertification program you may be most familiar with is the CPC Program.
The CPC Program consists of two 4-year cycles, totaling 8 years.
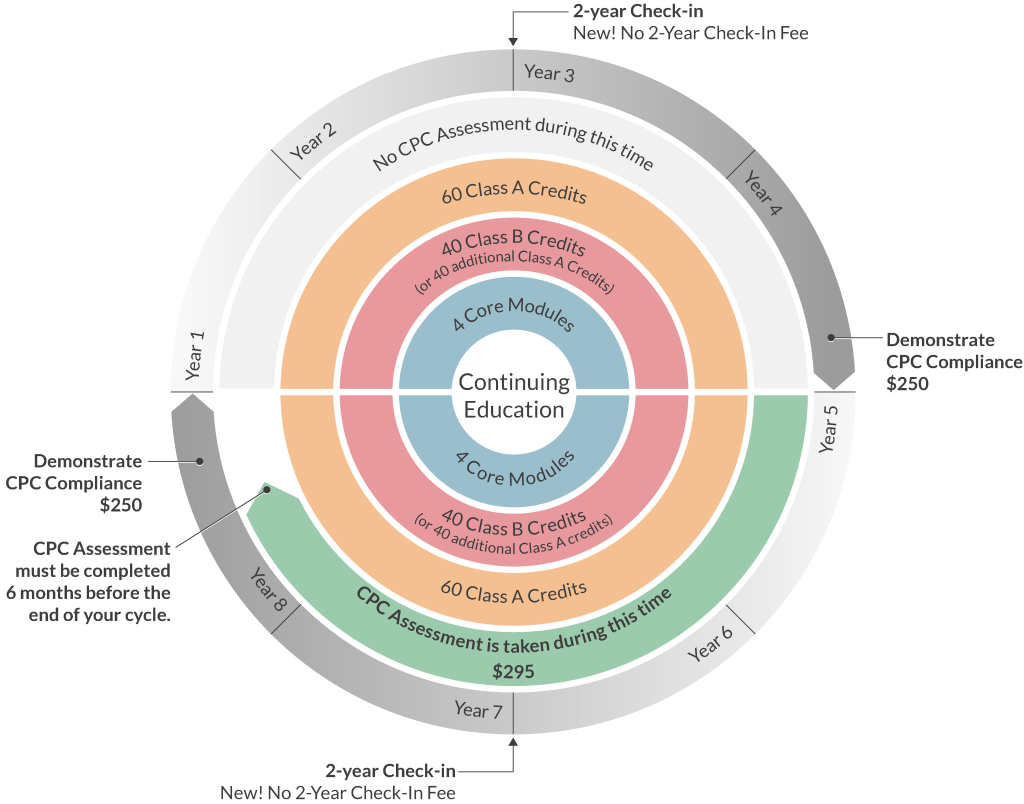
In the first 4-year cycle, CRNAs complete:
- 60 Class A credits
- 40 Class B credits
- CPC Core Modules
- Airway Management
- Applied Clinical Pharmacology
- Physiology/Pathophysiology
- Anesthesia Equipment and Technology
In the second 4-year cycle, CRNAs complete:
- 60 Class A credits
- 40 Class B credits
- CPC Core Modules
- Airway Management
- Applied Clinical Pharmacology
- Physiology/Pathophysiology
- Anesthesia Equipment and Technology
- CPC Assessment
Each cycle requires a midpoint check-in where you must validate your state licensure, confirm active practice, and update your contact information with the NBCRNA.
At the end of each 4-year cycle, you’ll log into the NBCRNA portal to complete your application and pay the fee, provide documentation of current licensure, demonstrate you’ve completed the CPC Program, and submit a record of anesthesia practice.
CPC glossary: What you need to know about the requirements
Class A Credits
Class A credits can be earned by completing continuing education courses, webinars, and Core Modules. They must have prior approval by the American Association of Nurse Anesthesiology (AANA) and include an assessment.
Class B Credits
Class B credits can be earned by various methods including conducting research, teaching, publishing, and more. Check out our Guide on CRNA Class B Credits to learn more. You must keep an accurate record of these credits as they don’t require prior AANA approval or an assessment. You can also earn additional Class A credits after completing the required 60 to satisfy your Class B requirements.
CPC Core Modules
The CPC Core Modules are specialized Class A credits that teach up-to-date, evidence-based practice trends in the four domains of CRNA practice. Although CPC Core Modules aren’t required for the MAC Program, they’re an efficient way to stay at the forefront of anesthesia practice while earning Class A credits.
CPC Assessment (CPCA)
The CPCA is a three-hour, 150-question assessment. You must complete the assessment for CRNA recertification, but it is not a pass-fail exam. It’s a tool to measure your knowledge, and your results will help you identify focus areas for additional study.
How to earn CRNA continuing education credits
Meeting your CRNA continuing education requirements is simple with the right resources. Whether you’re in the CPC Program or MAC Program, APEX offers convenient, cost-efficient bundles to support your recertification.
As CRNAs, we understand how challenging it can be to fit CRNA continuing education credits into your busy schedule. That’s why our online courses are available anytime, anywhere, and award Class A credits, meeting the CPC Program Standards as well as the MAC Ed and MAC Dev requirements.
We’re here to help you on your CRNA recertification journey. Choose a bundle that works best for you today.
Before we talk about the future of anesthesia, let’s look back at how things change. Change can come slowly or with astonishing suddenness. If you were training or practicing—or know of someone who was—in the early 1980s, the anesthetic recipe might very have involved:
- Thiopental for induction
- Halothane and nitrous oxide for maintenance
- Meperidine, morphine, or fentanyl for analgesia
- Laryngoscope
- Innovar (a fixed combo of fentanyl & droperidol)
- Succinylcholine, curare, or pancuronium for relaxation
- Manually inflated BP cuff, ECG, nerve stimulator (maybe)
- Pneumatic-powered anesthesia machine
- Black rubber breathing circuit and Ohio mask
- Pen and paper charting
While a few items have survived the cut, consider what’s missing from the list, interventions that are now staples of contemporary practice. Today we have sevoflurane, propofol, rocuronium, dexmedetomidine, oscillometric BP, pulse oximeters, infrared agent analyzers for carbon dioxide and our potent inhaled agents, accelerometers, video laryngoscopes, and ultrasound devices. You get the message, change is a constant.
Table of Contents
- Star Wars, Doug Quaid, Tony Stark, and many others!
- Besides being entertaining, what does all that have to do with us?
- Predicting what will (might) happen to our patients
- Important questions to ask with no easy answers
- The past is what you’ve done – the future is what you have learned
The acceleration of technology and knowledge in our specialty continually creates—at an astonishing pace—additive and synergistic applications of innovative devices, new approaches, and how we interact with our patients. Throw in a large dose of human inventiveness, entrepreneurial spirit, industrial competitiveness, open-minded regulators, and what’s happening in popular opinion, what seems like futuristic thinking may already be knocking on our door.
Star Wars, Doug Quaid, Tony Stark, and many others!
The motion picture industry can conjure magical moments that later appear in real life. We love films, and with the theme of visionary technology, consider just a few of our favorites:
- Video calling is displayed in the 1927 film Metropolis.
- One of the “smartest” sci-films of all time, The Day the Earth Stood Still. This 1951 film’s robot, Gort, may be the first true artificial Intelligence (AI) in the history of motion pictures.
- The 1968 film 2001: A Space Odyssey depicted a fully functional tablet and machine learning (ML).
- Dick Tracy’s smart-watch, in 1946, ok, not a film, but we like comic strips too!
- Autonomous cars, 1990, in Total Recall.
- And oh, so many more!!!
Now think of the original Star Wars, where the ever-resourceful R2-D2 creates a hologram of Princess Leia requesting help from Obi-Wan Kenobi. And what about the first Total Recall film, where Doug Quaid (future governor of California Arnold Schwarzenegger!!) uses his watch to project a full-body holographic image of himself into a previously empty space?
Then we have Tony Stark (Robert Downey, Jr.) in Iron Man 2, where holograms are extensively used, providing him with superhuman capacities to invent, analyze, and utilize them as centerpieces in the film.
Besides being entertaining, what does all that have to do with us?
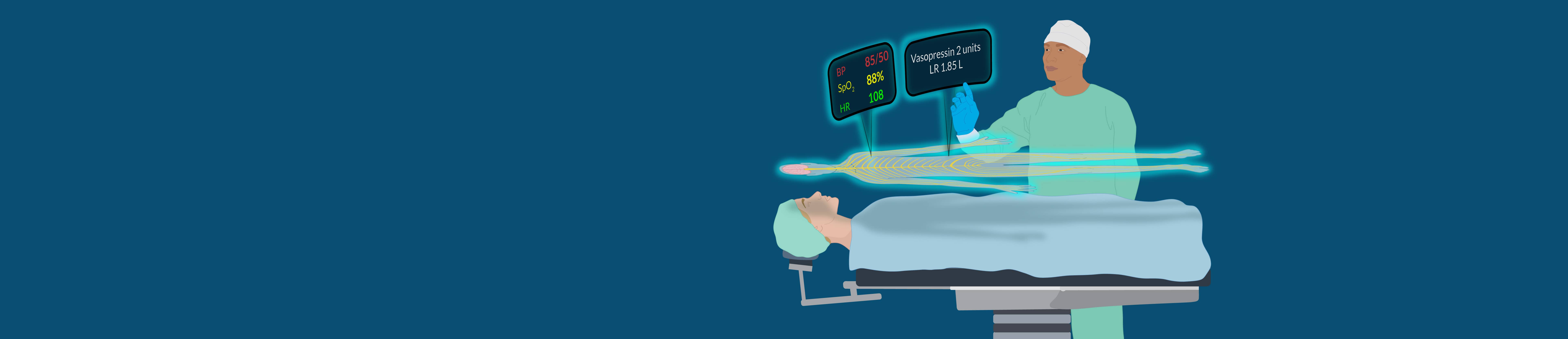
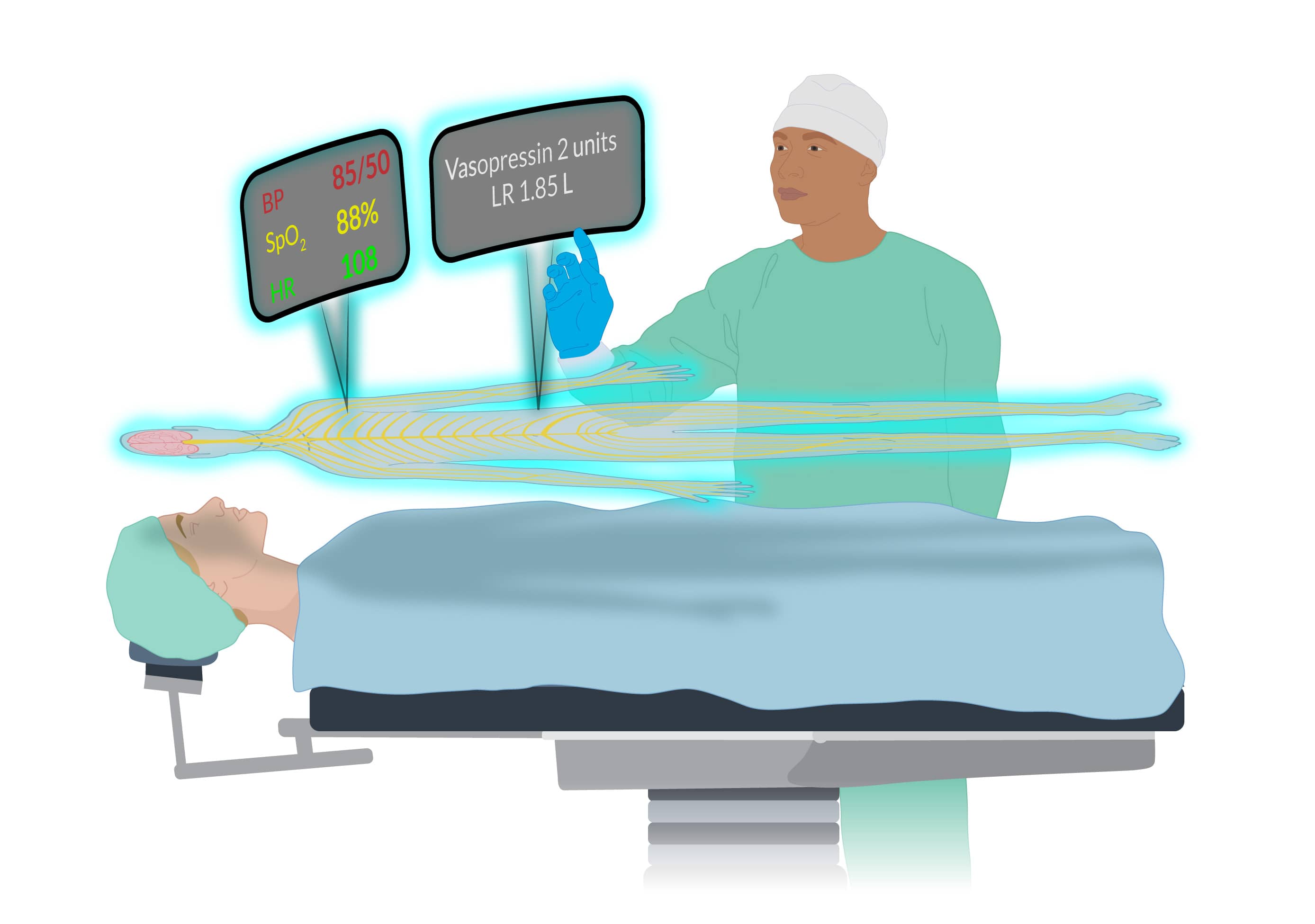
The technology company IKIN has created remarkable 3D holographic devices that project holographic content in color and ambient light in a large format. Their approach allows the human side of the interface to enlarge and manipulate projection elements without the need for goggles. Euclideon, an Australian tech company, uses a similar approach. The RYZ Holographic System™ seeks to optimize and maximize the technology’s applications.
There is no shortage of interest in the field, with companies with intriguing names like Vivid Q, Haloxica, HyperVsn, and many others aggressively developing their approaches. The company Humane, an AI-intense entrepreneurial effort, has patented technologies that use laser projections, three-dimensional cameras, and biosensors. And let’s not forget what Apple, Amazon, Google, Microsoft, NVIDIA, Tesla, and Meta may be up to! Many of these technologies have yet-to-be-defined targets, and they are quietly pursuing applications of these and offspring that may replace the computers, smartphones, and smartwatches we currently use.
Exactly how this will play out in healthcare, specifically in the CRNAs’ milieu where the display, analysis, and management of physiological data are key to what we do, requires clarification. But what we see in movies, where holographic images and icons hang in the air for protagonists to manipulate—well, that “fantasy” may be a lot closer to our reality than we might think.
Predicting what will (might) happen to our patients
It’s not all speculative science fiction that is shaping our future workplace. In some ways, the future of anesthesia has already arrived with what may best be characterized as a punctuated evolution. Many new initiatives are focusing on innovative monitoring that guides clinical decisions to:
- Maintain or improve brain health
- Avoid failure-to-rescue (FTR)
- Lower the risk of acute kidney injury
- Reduce MINS (myocardial injury after noncardiac surgery)
- Lessen postop opioid use disorder
- Reduce the risk of cardiac arrest
A batch of approaches are in the works or already with us termed medical early warning systems (MEWS) designed to assist us in recognizing warning signs of a deteriorating patient before human identification. The general view is that these will become commonplace throughout our specialty, not only in the OR, but also in the PACU, ICU, and postop hospital wards. MEWS can warn us about the implications of what might only be a subtle, easily overlooked change in a patient’s condition and predict conditions like hypoxemia, hypotension, embolic issues, metabolic disturbances, and neurological insult. This is based on exquisite, real-time monitoring of key physiological parameters with ongoing AI or ML integration.
The Edwards’ Hypotension Prediction Index is an existing system with a research and clinical track record. It uses machine learning to predict intraoperative hypotension before it happens.
This is complicated stuff. It is not just about measuring HR and BP but rather using biosensors to collect and integrate data that might include breathing patterns, cognitive function, genetics, body position, stress level, infection risk, level of consciousness, biomolecules, and other factors limited only by our imagination.
A British Journal of Anaesthesia paper recently demonstrated an AI platform’s keen ability to use intraop data analysis to predict postop hypotension. Another fascinating paper in Nature Reviews Bioengineering, revealed the uncanny ability of an AI tool called ‘Prescience,’ to forewarn of hypoxemia. The key theme in all these technologies is looking beyond the immediate at what may be coming.
Consider that there is a well-recognized 10-30% in-hospital risk of patients experiencing dangerous postop complications. Continuous postop surveillance monitoring systems, aided by AI, can decrease the risk of failure-to-rescue events by predicting which patients might deteriorate before clinical evidence appears. Integrating AI and ML with existing monitoring strategies can detect patterns of subtle, nuanced changes in patient parameters that providers will likely overlook.
Important questions to ask with no easy answers
Let’s finish by asking questions relevant to CRNAs and all healthcare workers. While we do not presume to have all the answers, we hope to get you thinking about some of the implications of new technologies.
What potential does healthcare technology have for patient care?
It will be revolutionary as AI allows us to access, analyze, and apply superhuman amounts of data to diagnostic and healthcare decision-making at speeds, with certainty (errorless), and at lower cost than what a human alone can muster.
What limits are envisioned for healthcare technology?
Besides immediate application to patients, AI, and virtual reality will be increasingly used in teaching, diagnostics, problem-solving, and administrative tasks. That is, they have no limits. Biosensor technology is rapidly growing. Miniaturized autonomous sensors will be self-learning and never need maintenance, as they will be self-calibrating.
What are the challenges that new technologies create?
Data security and integrating new technology with that currently used will pose problems. As many of us have seen with EMRs, its incorporation into the institution’s existing platforms is rarely seamless. Also, who pays for these technologies, and what are their environmental impacts?
The past is what you’ve done – the future of anesthesia is what you have learned
Consider the original anesthetic recipe we presented at the start. In the early 1980s, the risk of dying from anesthesia was 1:10,000; today, it’s almost unmeasurable in ASA 1-3 patients. Advances in technology play an enormous role in enhancing the safety of our work.
Allow us to speculate. In the not-too-distant future, you may voice activate a hologram powered by AI to consult with an expert in real-time as you care for a patient. A synthesis of data gleaned from myriad biosensors displayed in a user-friendly interface will be available to you. With finger or voice activation, you have immediate access to all the world’s published information relevant to the patient you care for.
This all may be closer than you can imagine. Yet that’s just it, as our imagination is the driver behind all of what is coming.
As CRNAs ourselves, we understand the challenge of fitting CRNA continuing education credits into your busy schedule. When you’re ready, we’re here to help.
If you’re a nurse anesthetist in the Continued Professional Certification (CPC) or Maintaining Anesthesia Certification (MAC) Program, you’re in the right place. Regardless of the program you’re in, the National Board of Certification & Recertification for Nurse Anesthetists (NBCRNA) requires you to complete 100 hours of continuing education and professional development, including 60 Class A credits and 40 Class B credits. We understand it can be difficult to earn these credits with a busy lifestyle. That’s why we’ve created a one-stop shop for everything you need to know about CRNA Class B credits.
Table of Contents
What are Class B credits?
Class B credits are a type of continuing education nurse anesthetists are required to earn for recertification. Unlike Class A credits, Class B credits don’t require AANA approval, have an assessment, or undergo a prior-approval process. Whether you are enrolled in the CPC or MAC program, you must earn 40 Class B credits per four-year cycle.
How to earn Class B credits
Qualifying activities for CRNA Class B credits must meet one of the following criteria:
- Enhance knowledge of anesthesia practice
- Support patient safety
- Foster an understanding of the broader healthcare environment
From teaching to mission trips, there are various activities that qualify as Class B credits. They include:
- Class A: Assessed Continuing Education (CE)
- Subspecialty or Austere Clinical Practice Role
- Non-Prior Approved and/or Non-Assessed CE
- Integration of a New Clinical Practice Technique
- Academic Credits
- Service – Seated or Elected Activity
- Presentations
- Service – Mission or Diplomacy Activity
- Publication – Book
- Service – Advocacy or Public Relations Activity
- Publication – Chapter
- Life Support Courses
- Publication – Peer Reviewed
- Quality Improvement Initiatives
- Publication – Grant
- Discovery
- Teaching in the Clinical Setting
- Research or Practice Inquiry Project – Member of Committee or Team
- Clinical Administrative
- Research or Practice Inquiry Project – Principal Investigator or Individual Completion of Dissertation, Thesis, or DNP/DNAP Project
Earning Class B credits from Class A credits
If you earn over the required number of 60 Class A credits, you can roll those over to count towards your Class B requirement. With APEX Anesthesia Review, you can fit earning Class A and Class B credits into your busy schedule. Get everything you need for your 4-year cycle with one of our CRNA continuing education bundles, which include hundreds of AANA-approved Class A credits delivered in multiple methods and are more than enough to cover your Class B credits requirement.
Class B credit documentation
Each Class B category has a required audit document you’ll need to keep on file. There is also a category reporting document you can download. View the NCRNA Class B table to see the corresponding documents to keep a record of.
Maintaining your activity records is essential for reporting Class B credits in your credential renewal. Even though the NBCRNA has an honor system, they may still audit you for your corresponding documents.
One of the key benefits to applying excess Class A credits to your Class B requirement is that APEX will save you time and give you peace of mind by reporting these credits to the AANA for all active members.
Submitting Class B credits
If you’re an active American Association of Nurse Anesthesiology (AANA) member, you can record and track AANA Class B credits as well as submit documentation on the AANA website. Not an AANA member? You’ll need to report your Class B credits during your 4-year credential renewal. If you’re not an AANA member, you’ll report your Class B credits to the NBCRNA.
Using APEX for your NBCRNA Class B credits? Perfect! APEX reports credits for active AANA members during business hours Monday through Friday, saving you the extra step of submitting Class B credits yourself. If you’re not an AANA member, you can also print your APEX credit transcript to submit to the NBCRNA.
APEX makes it easy to get everything you need for your entire 4-year CPC cycle or MAC cycle! Ready to get started? Check out our courses for CRNA Continuing Education credits.
There is an undercurrent of neuroscience-grounded activity underway in our professional community. Niches of CRNAs nationwide, working alone or in concert with like-minded physicians, are challenging some of the historical and contemporary foundations of general anesthesia. Largely quiet in their activities, representing a very small circle inside a much larger circle on a Venn diagram, they are pursuing their ambition to eliminate the use of potent inhaled agents in their practices and turning to total intravenous anesthesia (TIVA).
Table of Contents
- What we learn about general anesthesia in our basic programs
- Targeting specific receptors and an introduction to our term, “C-FAN”
- The downsides to potent inhaled agents
- The emergence of clinician-friendly measurements of CNS activity
- C-FAN is not a processed EEG!
- Should our ether hybrids be abandoned?
While rubrics like “radical,” “maverick,” or “intrepid” come to mind, these fall short of singularly capturing the mindset, passion, intellect, and purpose of these devotees. For now, we will dispense with labeling them; instead, leave that up to you as we describe just what these clinical practitioners and thinkers are up to.
What we learn about general anesthesia in our basic programs
Let’s journey back to your early training days when you first truly appreciated what general anesthesia was all about. Regardless of your vintage, you likely learned a contemporary descendant of an ether-based compound brought it on. We’ll give a quick shout-out to halothane (an alkane), but otherwise, we’ll confine our discussion to the three halogenated ethers in current use—isoflurane, sevoflurane, and desflurane.
You came to know that ether-based anesthetics are “total” anesthetics. In a dose-dependent manner, they produce unconsciousness, amnesia, analgesia, areflexia, and akinesia, collectively representing the required components for a general anesthetic state. Miss one of these targets, and oops, something important is missing. But in the case of our current ether hybrids, one drug does it all.
These clinical goals are not achieved with a uniform dose; each pharmacological target demands a specific concentration at the respective effect site. The dose of sevoflurane needed to achieve akinesia differs from that required to produce unconsciousness, and so forth. One MAC of an agent fails to address the individual components of general anesthesia and only gives us an overall potency metric in preventing purposeful movement to a nociceptive stimulus like a skin incision. Achieving a particular clinical target with a potent inhaled agent may result in unacceptable hypotension.
Targeting specific receptors and an introduction to our term, “C-FAN”
We circumvent this limitation by using what some refer to as “balanced” anesthesia (old-timers may prefer “garbage anesthesia”), in which we add specific drugs targeting unique receptors that mediate the precise response we want. Nicotinic, muscarinic, GABA, NMDA, 5-HT3, and alpha-2 receptors, among others, come to mind.
We have two broad approaches to achieving a general anesthetic state: inhalational and TIVA. Both are safe, titratable, and effective. These approaches have been with us for a long while, with the inhalational approach having about a century’s head start! But what’s happened over the last 25 years is a systematic and methodologically sophisticated understanding of what’s going on grounded in what we term “Clinician-Friendly Actionable Neuroscience,” or, for simplicity, C-FAN.
Googling C-FAN, you’re not going to come up with anything as it’s a term we created, and currently, it’s more of an evolving idea than a thing. We’ve only now put it out there for others—like you—to consider. So, what’s going on here, and what’s up with C-FAN?
The downsides to potent inhaled agents
First, there are a lot of concerns about traditional, potent inhaled agents. Among these are that in animal models and even in some human observational studies, there are concerns that general anesthesia induced by our potent inhalants may have neurodegenerative effects. Some suggest that these effects may be particularly concerning in young children (subsequent learning impairment, attention deficit disorder, behavioral issues) and older adults (cognitive impairment), prompting an FDA warning that’s just a hair shy of a boxed warning. The literature also suggests a high incidence of emergence delirium—acutely or in the first hours or day or so)—in pediatric and adult patients.
There are also concerns that long-term occupational exposure to even trace amounts of these agents may have biological consequences for us and other members of the operative team. Added to this is the now well-appreciated contribution that the potent inhaled agents have on greenhouse gases and their deleterious effects on the ozone level when they are vented to the outside air ending up in our atmosphere. Some even suggest they play a consequential role in what is described as global warming. Then there is the issue of cardiovascular depression, often caused by incidental overdosing to achieve a desired state with attendant adverse events like acute kidney injury.
These issues are widely discussed in the literature and have gained traction in the minds of some providers who, armed with C-FAN, have sought alternatives. These forward-thinking, early adopters of TIVA, to the point of eliminating potent inhaled agents from their practice, come grounded in what they believe is an evidence-based, practical, safe, and highly effective respite from inhalants. They’ve become iconoclasts with total avoidance of the potent agents from their practices. Their view is to use the tools and understanding that neuroscience offers to employ precision medicine in their clinical care of patients.
The emergence of clinician-friendly measurements of CNS activity
There is a bit of an irony that everything we’ve ever seen and know about life on planet Earth comes to us from an organ that resides in an encapsulated enclosure devoid of light. Its matrix is such that if you were to scoop it out of its enclave and hold it in your hands (use both, or you might drop it!), you’d perceive it as feeling a bit—on the “tofu scale”—as middling between regular and firm. But continually coursing through this extraordinary organ, via its neuronal circuitry, is an inconceivably large flood of electrical activity. That activity can be captured by now common and relatively compact devices that display the electrical activity permitting clinician analysis, and providing a real-time opportunity to achieve targeted outcomes pharmacologically.
The entire May 15, 2024 issue of Neuron, a high-impact journal, is devoted to clarifying what consciousness is and how unconsciousness is induced. Using easily acquired electrical signaling, MIT researchers revealed that disrupting the brain’s normal balance between stability and excitability makes its activity increasingly unstable until unconsciousness ensues. The researchers note that the brain operates on what might be termed a “knife’s edge” between excitability and chaos. It must be excitable for neurons to interact with each other, but if it becomes too excitable, chaos can rule.
This research underscores the value of using and analyzing specific electrical patterns induced by drugs such as propofol or those targeting the other receptors mentioned earlier. It offers a pathway to developing ways to control a patient’s level of anesthesia more precisely.

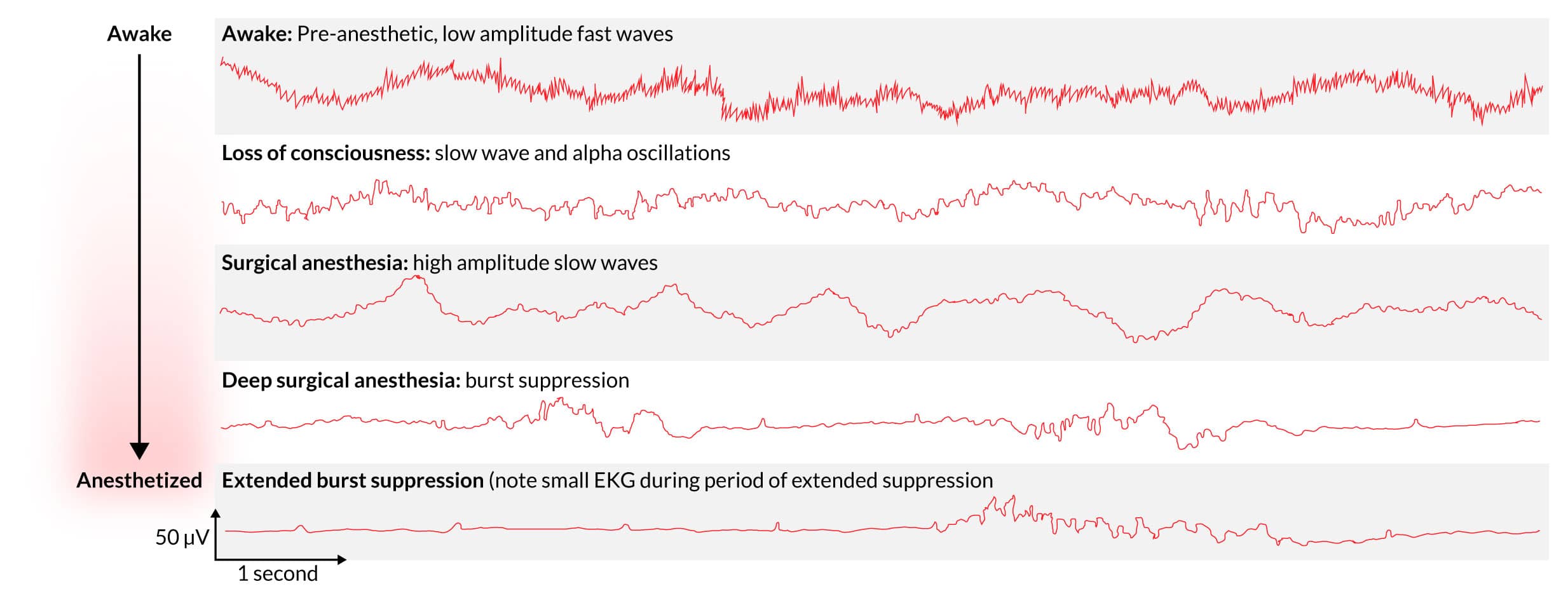
The foundations for these TIVA devotees come from a large body of bench and clinical research grounded in neuroscience, a field of biology that is only now beginning to receive its due recognition in our domain. What we now know is that:
- When humans “go under” general anesthesia, the brain is hardly “turned off” but rather pulses with dynamic electrical activity
- The drugs we use alter our normal arousal by inducing and maintaining oscillations in electrical activity.
- The activity is easily captured and observed with electroencephalography (EEG) acting like a simple voltmeter.
- The oscillations have “signatures” that permit tracking of the anesthetic state.
- A drug like propofol, or sevoflurane, acting on the GABA-A receptors allows negatively charged chloride ions to enter the cells of the CNS and quiet them–observable with that voltmeter.
- The oscillations change as the anesthetic depresses the CNS, with characteristic waveforms occurring.
- The waves initially get bigger, with slow oscillations revealing a depressed brain stem. Finally, burst suppression reveals a profound state of brain inactivation.
What is happening is some of these early adopters propose a new and enlightened, neuroscience-based approach to brain monitoring of patients receiving general anesthesia or sedation. They propose to train CRNAs to recognize and analyze anesthetic-induced brain states with drug-specific neurophysiological signatures gathered with an unprocessed 4-channel EEG and a spectrogram. Achieving and monitoring a desired anesthetic state using these unique signatures mirrors the molecular and neural circuit mechanisms of the activity of our drugs.
The ability to make detailed and accurate determinations is advocated by these aficionados as a way to optimize our ability to hit targets precisely and design patient-centric anesthetic care using a multimodal approach. They emphasize precise control of antinociception and simultaneously advantage the precise pharmacokinetics as the patient is controllably aroused from anesthesia.
In 2024 many envision raw EEG monitoring becoming commonplace in monitoring drug effects and see multimodal TIVA as a neurophysiological way to combine, control, and optimize the delivery of the agents. This permits second-to-second targeting of anesthetic depth and exacting control over the speed of emergence, with the hope of decreasing the adverse effects of the potent vapors.
C-FAN is not a processed EEG!
There are now compact, battery-powered EEG monitors, wireless with comfortable and adjustable headsets that leave no residue. This is not a BIS monitor or other proprietary-based, processed EEG device prone to measurement and interpretive pitfalls. C-FAN uses a raw EEG that is easy to use and interpretable with minimal training for the CRNA to gain the facility for its interpretation sufficient to guide precision TIVA. Proponents argue this technology is like moving away from auscultating BPs to automated noninvasive BP determinations, etCO2 replacing arterial blood gas analysis, and pulse oximetry supplanting indirect clinical estimations of arterial oxygen content. CRNAs use highly sophisticated technologies with aplomb—think ultrasound guidance for nerve blocks, line placements, and many other assessments. Our technological skill sets also include cardiac ECHO, TEE, quantitative neuromuscular function monitoring, and advanced ECG interpretation. Simplified EEG analysis is likewise on the horizon, and sufficient mastery is highly achievable.
C-FAN is neuroscience marshaled to the patient’s bedside, precisely using a cocktail of agents, including IV propofol, short-acting analgesics, drugs that create akinesia, and others that target specific regions of the brain, like ketamine and dexmedetomidine. This provides an alternative to inhaled agents using raw 4-channel EEG signals captured in real-time with C-FAN-friendly tools. The site of action of our anesthetics is the CNS; we should and can specifically target the effect site using emerging technologies. And once AI gets pulled into the picture, its use will be even more actionable.
Should our ether hybrids be abandoned?
No!! We are not advocating for eliminating these time-tested, reliable, and titratable members of our pharmacopeia, nor are we suggesting that TIVA is optimal for all cases and practices. We are reporting on what appears to be an undercurrent of clinical practice that is growing domestically and internationally. C-FAN monitoring tools are coming our way just as 1973 heralded the first use of the cell phone and the avalanche of technology that it foretold.
Does this represent an existential threat to “traditional” general anesthesia induction and maintenance? Or is it just the ever-evolving nature of what we do? It may be coming to an OR close to you if not already there.
As CRNAs ourselves, we understand the challenge of fitting CRNA continuing education credits into your busy schedule. When you’re ready, we’re here to help.
Considering Internet traffic, lay publications, and peer-reviewed clinical studies, parents are confronted with the angst that their young child’s brain, undergoing surgery, may experience neurocognitive toxicity due to our anesthetic drugs. It is a natural next step to ask about the potential risks pediatric general anesthesia poses for the developing brain. How should CRNAs address their concerns?
Table of Contents
- The FDA sent out a warning
- The remarkable human brain and all those neurons
- Neurotoxicity – a concern in the age of wobbly information
- Major outcome studies in pediatric neurotoxicity
- Explaining pediatric general anesthesia risks to anxious parents
In the March 2022 issue of the journal Anesthesiology, a paper by prominent voices in pediatric anesthesiology entitled “Anesthesia and developing brains: unanswered questions and proposed paths forward” appeared. Another paper of equal stature in the icons of medical science from across the Atlantic Ocean, the British Medical Journal, asked, “Does general anesthesia affect neurodevelopment in infants and children?”
Along the way, also from across the pond, a disturbingly worded paper appeared in the British Journal of Anaesthesia: “General anaesthesia, the developing brain, and cerebral white matter alterations.”No one likes having their brain “altered,” so the possibility reflected in the title gave us a modicum of angst.
The FDA sent out a warning
These recent works come to us after a concerning December 2016 FDA Drug Safety Communication. This was a formal warning that anesthetics that bind to GABA and NMDA receptors used in those younger than 3 years old and pregnant women during the 3rd trimester may negatively affect the child’s brain. The warning was repeated later with somewhat more concerning language, which we truncate for brevity:
The FDA is notifying the public of changes in our previous warning about the use of general anesthetics in children, these include:
- Exposure to these medicines for lengthy periods of time or over multiple surgeries or procedures may negatively affect brain development in children younger than 3 years.
- Additional concerns about pregnancy and pediatrics describe animal studies that show exposure to general anesthetic and sedation drugs for more than 3 hours can cause widespread loss of nerve cells in the developing brain.
The warning involves at least 11 drugs we commonly use that bind at GABA or NMDA sites, including all anesthetic gases and our IV agents propofol, benzodiazepines, ketamine, and barbiturates. And we are not only being “warned” about using drugs affecting multiple receptors in young children but also in patients during their third trimester. If this is the case, one is left to wonder if there should also be a concern during the second or even the first trimesters. We get this issue with synaptogenesis, but if there is a legitimate concern, should it be broader? How much, or rather how little do we actually know?
The remarkable human brain and all those neurons
The human brain is wondrous, composed mostly of water (~75% by weight), and everything else being fat or protein. When removed from its bony enclave at fresh autopsy, it feels like soft tofu in one’s hands (which we have done; we advise using both hands!). As described to us by neurosurgeons, a bit of brain cortex about the size of a grain of sand may contain over 50,000 neurons, each creating well over 5,000 synapses. With almost 20% of the cardiac output going to the brain and a disproportionately large energy utilization, especially early in life, this organ is vital and darn expensive to run! The expenditure is so great in infancy that it may explain why infants generally sleep 14-20 hours each day!
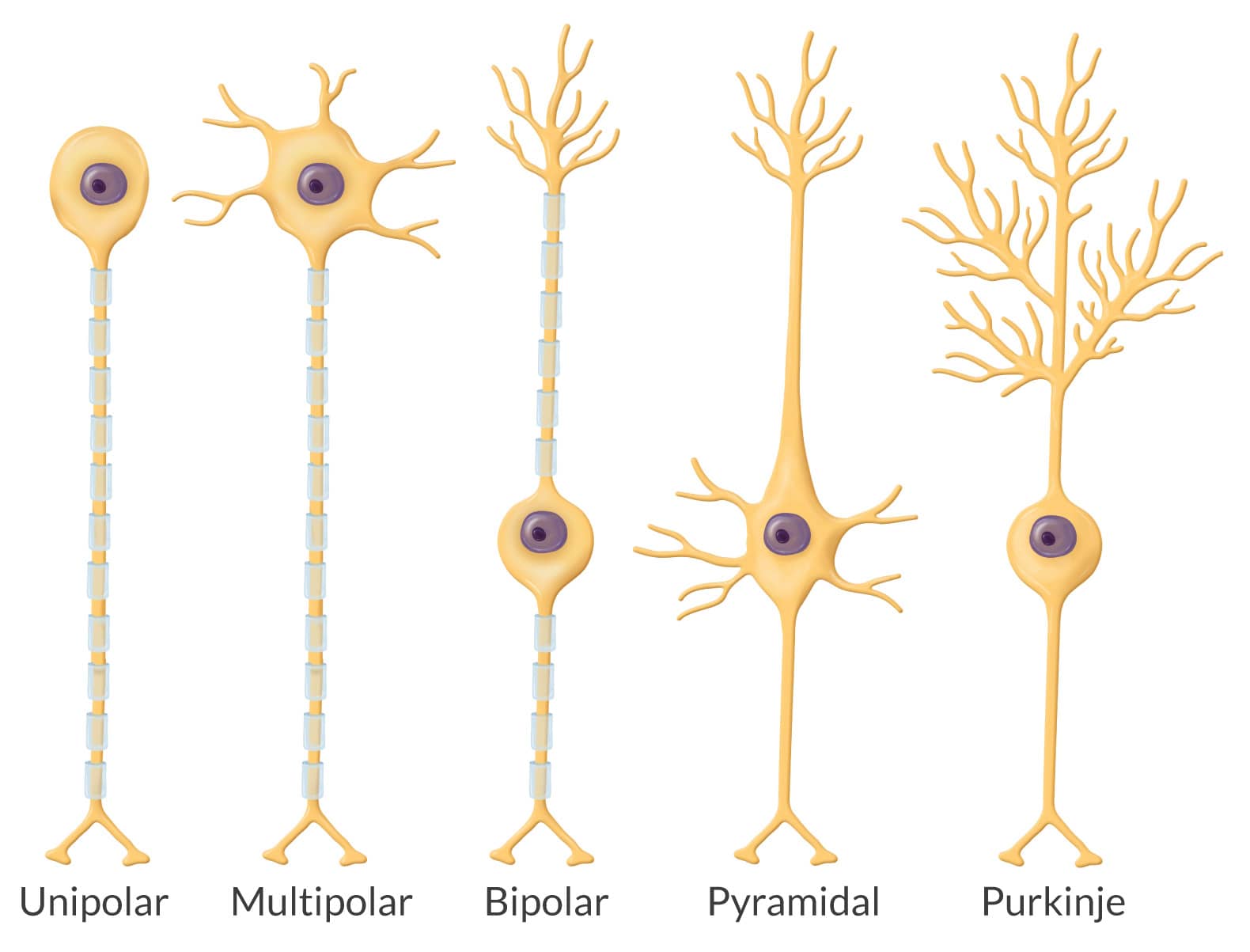
A neuron is unlike anything anywhere else in the body. Neurogenesis and synaptogenesis start in “embryo-hood,” proliferating at a rate rivaling blood cell genesis, peaking in about 3-4 years. Adults may have 86 billion neurons of 5 different types: unipolar, pyramidal, multipolar, bipolar, and Purkinje. The cell body and its long axon with tiny telodendria at its end look alien, menacing, yet paradoxically vulnerable. With their dendritic extensions, our brains harbor trillions of synapses. While the adult blood-brain barrier keeps neurons safe, the young child’s barrier is immature and permissive to toxins.
Neurotoxicity – a concern in the age of wobbly information
When seeking relationships involving biological phenomena, it is common for some to suggest cause-and-effect relationships even though there may only be an association at work. In contrast, others find no relationship at all. The temperature in the room can rise significantly among providers (e.g., CRNAs) and policymakers (e.g., the FDA) when discussing the risks and benefits of pediatric general anesthesia. For example, many hold tenaciously to one view, with little potential to move the needle even when reasonable contrary evidence is brought to the debate.
It is now common, armed with information and disinformation that spreads instantly and widely across the Internet with a single keystroke, for parents to ask if our anesthetic will harm their young child’s brain. They’ve likely heard of the FDA’s warning, with many having thoroughly researched it. What should we say to an anxious parent?
Major outcome studies in pediatric neurotoxicity
The first preparatory step is to consider the literature. Besides the risks demonstrated in animal studies, let’s briefly consider a few of the more prominent and elegant studies on humans performed worldwide:
- GAS (General anesthesia vs. spinal in young children). Here, 722 infants in over 20 centers worldwide who underwent inguinal herniorrhaphy were randomized to receive sevoflurane or an awake spinal anesthetic along with a sugar-coated pacifier. There was no difference in neurobehavioral outcomes at age 2 or 5 years.
- MASK (Mayo Anesthesia Safety in Kids). Neurobehavioral testing was performed in 411 controls (no anesthetic), 380 had one anesthetic, and 206 had multiple anesthetics. There was no difference in IQ testing among the groups, and processing speed and fine motor function were decreased slightly in those who received multiple anesthetics. Parents of those receiving multiple anesthetics reported more behavioral issues.
- Avon Longitudinal Study of Parents and Children. This prospective study grouped 13,433 children by none, one, or multiple exposure to general anesthesia before their 4th birthday. Motor, cognitive, language, educational, and social assessments were performed at ages 7 to 16 years using school exams, parent/teacher questioning, and in-person visits. There was no evidence of clinical neurotoxicity, but poorer motor and behavioral issues were seen in those exposed to multiple anesthetics.
- PANDA (Pediatric Anesthesia Neurodevelopment Assessment). To control for genetic factors, this crafty study published in JAMA, included children younger than 3 years who were siblings, one of whom had one anesthetic exposure, the other who had no exposure. Follow-up was at 8 and 15 years assessing neurocognitive function. All 105 sibling pairs were ASA I or II and no neurocognitive differences were found between the sibling pairs.
- Columbia University Longitudinal Study. Using Texas (25,855 children) and New York (16,843 children) enrolled in Medicaid, matching pairs, similar in attributes and all <5 years, were grouped by those who received one general anesthetic and those unexposed. Using ADHD medication prescriptions as the outcome, those receiving anesthesia were 37% more likely to require persistent drug treatment for ADHD.
Getting at the ‘truth’ regarding anesthetic-induced neurotoxicity–if there even is a single ‘truth’ –is dauntingly complex. It’s like attempting to quantify biodiversity. The National Geographic Society reports over 8 million species on Earth, yet only about 1.2 million have been identified. The task is Sisyphean in nature, as even the definition of “species” is in flux. The deeper one looks, the more jaded a single ‘truth’ becomes. Such is the case with anesthetic neurotoxicity, where trying to separate direct drug effects from comorbidities, inflammation, hypo- or hyperoxia, dysthermoregulation, pain, surgical trauma, nutrition, and illusive genetic influences greatly complicates definitive conclusions. There is also the nontrivial factor of drug dose and the timing of exposure relative to the child’s development.
Then we must ask, as with defining a species, what exactly constitutes a neurotoxic outcome? ADHD? Lower IQ? Slower reading comprehension? Poor social behavior? Parenteral perception of the child’s interactivity? The challenge to arriving at an absolute truth is considerable.
Explaining pediatric general anesthesia risks to anxious parents

Approximately 2 million pediatric patients undergo general anesthesia each year, a good portion of which are < 1 year of age. The risk involved in requiring general anesthesia is wedded to the individual child’s attributes and their procedure. Based on the many studies available, the concern is extremely low for a relatively healthy 3-year-old having surgery lasting less than 3 hours; the risk being virtually unmeasurable for one brief anesthetic. Concerns about neurotoxicity with general anesthesia and surgery increase somewhat when the exposure exceeds 3 hours and the child has undergone more than one anesthetic. The primary concerns are a higher incidence of ADHD, mild learning deficit, and behavioral issues. As is usually the case, the surgery is necessary and time-sensitive, and postponement is unlikely, especially where congenital anomalies threaten well-being.
That said, available clinical research has changed many surgeons’ practices, with new information influencing the timing of surgical intervention. Reconstructive surgery, plastic surgery, certain urological, and other surgeries for conditions that do not immediately impair life and function are often postponed until the child is older. Some authorities express concern that the FDA warning may cause unnecessary delays in surgical and diagnostic procedures, paradoxically resulting in adverse outcomes.
Remember, like major league pitchers with more than just a fastball in their repertoire, we have options. Regional anesthesia, including neuraxial and area-specific blocks, is available in some settings and for some procedures that may obviate the need for general anesthesia entirely.
We want to end on a remarkable, brand-new, first-of-its-kind human randomized clinical trial design published in 2024 in The Lancet. It involved repeated general anesthesia exposures in vulnerable young children in the multi-site Australian Cystic Fibrosis Bronchoalveolar Lavage study. We believe this is an important study because it gets to the heart of a contentious, concerning, and lingering issue in pediatric anesthesia: the notion of anesthesia causing adverse neurocognitive and behavioral effects in the very young.
The methodology was robust and exacting and the paper underwent extensive critique by authoritative referees on both sides of the issue. We will leave you with the authors’ conclusions: “These findings suggest repeated general anesthesia exposure in young children …is not related to the intellectual quotient, executive function, or brain structure compared with a group with fewer and shorter cumulative anesthesia durations.”One expert reviewer suggested it’s time to stop chasing the ghost of anesthesia causing neurocognitive impairment.
Addressing parents’ concerns and questions about neurotoxicity—now part of the routine consent process in some institutions—should be evidence-based, empathetic, and reassuring; certainly, don’t be alarming! From the outset, parents face angst in deciding if their child should undergo surgery and anesthesia. Emphasize that their child is in exceptionally good hands and that your absolute priority is their child’s safety.
One of the APEX crew trained and worked for 4 years in a center where it was not uncommon to find yourself caring for patients who would be “under” for 10 hours or more. Cases approaching 20 hours were uncommon but not unheard of, and as a staff member, there was a very good chance you’d find yourself providing care for one of these challenging “long-haul” cases at some time.
The cases we speak of usually involved craniofacial reconstructions with many teams of specialty services, including pediatrics, neurosurgery, plastics, ENT, ophthalmology, maxillofacial, radiology, and anesthesiology providing care. Often, it involved craniofacial deformities—particularly memorable cases involved severe hypertelorism, with eyes so widely spaced it seemed the child would have to crank their head far to the left or right just to obtain a monocular view of what was straight ahead. In nearly every case, there were other congenital anomalies.
When considering the management of “long-haul” cases, we recall a paper in the Journal of Surgical Research that systematically analyzed the relationship between operative duration and complications across surgical specialties. The study revealed that complications increased with duration, approximately doubling with each operative epoch exceeding two hours. Metanalyses demonstrated a 14% increase in the risk of complications for every half-hour of additional time.
What’s this got to do with Mars?
There’s much talk these days about humans someday settling on Mars. This vision is strongly articulated by a polymath who makes cars, launches rockets, puts spy and communication satellites into semi-permanent orbit, and has engineered a cyborg-like interface to unlock human potential. This later enterprise, Neuralink™, involves nano- and neurotechnologies implanted as a brain-computer interface designed to translate one’s thoughts into action. It’s all heady stuff. But Mars?

Mars is a long (!!) way away. There is no single answer for how far Mars is from Earth because it all depends, as neither Earth’s nor Mars’ orbits are perfectly circular, and Earth orbits the sun at 67,000 mph while Mars clocks in at 54,000 mph. In August 2003, Earth was at its closest recorded distance of 34.8 million miles (we will not be this close again until 2237). When Earth and Mars are opposite the sun from each other, that distance is some 259 million miles. If we compute an average, a metric of little meaning without context, that’s way further than Earth is from the sun. No matter where Mars is relative to Earth, it’s very far away.
While a patient is under our care, we assume responsibility for all functioning systems, especially those we’ve pharmacologically incapacitated. We breathe for them, ensure oxygenated and nutrient-rich blood reaches their cells, assume mastery of their autonomic nervous system, control fluid balance, thermoregulate, blunt conscious and somatic sensations, and protect them from the ongoing surgical assault. The longer the case, the more demanding our tasks as we endeavor to ensure some degree of homeostasis. With reanimation, we want the patient minimally back to their preop baseline—in some cases, even better.
The challenges we face in providing such care grow and can multiply with each passing hour. We see in this a corollary, maybe even a metaphor of sorts for the polymath’s vision of establishing a living foothold on Mars when he stated, “we are less than 5 years away for uncrewed, less than 10 to land people, maybe a city in 20, but for sure in 30, civilization secured.” Thinking of the challenges of caring for a single patient for 5, 20 or 30 continuous anesthesia hours got us musing about the challenges of homeostasis and risk…….are humans up to the challenges of getting to and living on Mars?

You may think this is an odd juxtaposition of one’s thoughts. But let’s conduct our own gedankenexperiment, a Germanic word for the complex musings that Einstein engaged in, translated as “thought experiments.” While a bit of a stretch, the more we considered it, the more it all seemed to align with what we do when we care for a patient having a “long-haul” procedure. Consider some of the challenges we face in assuring homeostasis in the OR and then doing the same for those involved in a “long-haul” Martian venture—one that may be permanent. Let’s see where this takes us.
If living on Mars is the destiny of some, what are the “costs”?
This is a complicated question! The journey involves a daunting calculus, but what about long-term microgravity, cosmic radiation exposure, ubiquitous organ system effects, and being away from family and friends, maybe forever? What if something breaks? What about contingency plans? All are apt considerations, but there is more to consider—so much more.
Humans were not designed to accommodate anesthesia drugs; anesthetic drugs were designed to accommodate humans. One does not need to be a polymath to recognize that humans, without Sisyphean enterprise, cannot handle or accommodate space.
Let’s look, point-by-point, at some of the challenges of space flight and Mars colonization and see if anything along the way conjures up thoughts of a “long-haul” case you might have been involved in.
| “Long-haul” space travel risks | “Long-haul” anesthesia risks |
| Radiation exposure | Surgical trauma, drug mutagenicity |
| Hypoxic and harsh environment | Multiple hypoxic risks; cold; pathogens |
| Water & nutrient needs | Fluid balance, metabolic considerations |
| Microgravity effects | Effects of often extreme surgical positioning |
| Effects on brain, psyche | Short & long-term cognitive effects |
| Musculoskeletal, CV, vision, nervous system, and endocrine effects | Musculoskeletal, CV, vision, nervous system, and endocrine effects |
| Immunosenescence | Immune system impaired |
| High-risk enterprise | Moderate to high-risk enterprise |
| Extremely high cost | High cost |
It’s a fact that space flight alters human DNA. Radiation injury may very well be the single greatest concern, and methods to prevent it are elusive but essential. Studies from the Icahn School of Medicine at Mount Sinai, NASA, and elsewhere collected blood from astronauts who flew in the space shuttle over a 3-year period and found DNA mutations in all 14 studied astronauts. The concerns were an increased risk of cardiovascular disease and cancer.
International Space Station (ISS) astronauts spend a lot of time in space, averaging 4-6 months at a time, with a few spending nearly a year there. There are concerns that the cerebral vasculature stiffens in response to the microgravity of space with unclear consequences. Consider this, even after touchdown on Mars, if you weighed 150 pounds on Earth, you’d now weigh 57 pounds. Have you seen videos of astronauts coming off the space shuttle or ISS and needing help to walk? Changes in muscle physiology, the brain’s vessels, bone density, and blood circulation affect gait, neuromuscular physiology, and sensation.
Immunosenescence, neuroocular syndrome, and sarcopenia are major hits astronauts experience in microgravity. Space is not friendly to humans, and radiation exposure keeps returning to the top of the list of risk factors because it comes in a couple of ways. Naked protons emitted by that big fireball in the sky, critical to life here at home base, are of enormous but not the only radiation concern for space pioneers. So is the galactic cosmic radiation from other stuff that’s out there, like supernova events. Being in a capsule hurtling toward Mars and then landing there poses the potential for experiencing intense and protracted radiation exposure.
We must also consider the human psyche. Biosphere II, where 8 people lived for 2 years in what was supposed to be a self-sustaining enclosure, was plagued by multiple issues, including a failure to naturally produce enough oxygen, requiring an exogenous supply to be piped in. Food shortages and considerable psychological turmoil wore heavily on the biospherians, despite visits—separated by glass panels—from friends, family, and spectators. Isolation space travel for many months or years? The effects are unknown and perhaps unknowable until the venture unfolds. The learning will come in the doing.
The grand ecological experiment in the Arizona desert raised more questions than answers and cost over $200 million (in 1990s dollars) over its several-year lifespan. What’s the total cost of sending a team to live on Mars? Trillions of dollars.
We don’t mean to be naysayers—recall that just 6 decades ago, it seemed improbable to keep a patient safe under general anesthesia for “long-haul” times now routinely employed. Consider that a whole-face transplant at the Mayo Clinic may require as many as 30 hours of continuous anesthesia and surgical care. Human ingenuity and its plasticity can solve daunting problems. That vocal polymath who we alluded to earlier and those like-minded might be on to something! But it does give us pause.
As CRNAs ourselves, we understand the challenge of fitting CRNA continuing education credits into your busy schedule. When you’re ready, we’re here to help.
The most recent era of healthcare is personalized anesthesia, representing a movement from one-size-fits-all care to targeted, patient-centric therapies. Genomics is fundamental to this shift, defining what makes us unique from all others on Earth. Gene editing is among the most recently targeted therapies, an approach that may revolutionize healthcare. Let’s demystify the approach.
Table of Contents
- Innovative gene therapy
- The remarkable numerics of the human body
- A cautionary tale of the technology: Jesse Gelsinger
- Important questions to consider
- Gene therapy in personalized anesthesia—really?
- Where we are today
CRNAs who provide anesthesia care to those with sickle cell disease (SCD) know that there are life-threatening and debilitating effects of the condition. The sickling mutation causes red cells to assume a crescent (sickle) shape, leading to blood flow restriction and ischemic and vasooclusive events. Repeated, chronic ischemic events initially result in degraded quality of life, followed by often incapacitating disability and early mortality.
We worked for years in an institution with a preeminent SCD center and stayed abreast of therapies for this heritable disease. We were thrilled and intrigued when, in December 2023, the FDA approved the first two cell-based gene therapies, Casgevy and Lyfgenia, for the treatment of SCD.
Innovative gene therapy
Casgevy utilizes CRISPR/Cas9 technology, often referred to as “molecular scissors.” The discoverers of this technology were awarded the Nobel Prize in Chemistry in 2020. This process harvests a patient’s stem cells and modifies their DNA. The edited cells are then transplanted back into the patient, proliferating in the bone marrow and generating fetal hemoglobin (HbF), preventing sickling.
Lyfgenia takes a somewhat different approach. It uses a nonpathogenic virus to shuttle a genetic modification into the patient’s cells, where the gene therapy-derived hemoglobin is encoded and produced. This hemoglobin functions like adult hemoglobin (HbA) and is designated HbAT87Q.
Besides effecting a cure, a benefit of these innovations is that the process uses the patient’s stem cells, so immunological rejection is not a problem. A major drawback is that patients undergo initially debilitating chemotherapy to obliterate mutant cells from the bone marrow, which are then replaced by Casgevy- or Lyfgenia-modified cells. The treatments are also very expensive, with current estimates of Casgevy at $2.2 million and Lyfgenia at $3.1 million for each patient.
A wide range of side effects may occur, such as hair loss, infections, mouth ulcers, and, with Lyfgenia, possible blood cancers, necessitating its FDA Box Warning. Despite the side effects, these advances are considered significant medical breakthroughs with the potential to treat various conditions. Diabetes, rheumatoid arthritis, neurodegenerative conditions, and neuromuscular diseases come to mind. There are even forms of congenital blindness now believed to be amenable to gene therapy. We counted well over 100 diseases currently targeted with gene editing research and dozens of companies aggressive in their pursuit.
The remarkable numerics of the human body
Let’s digress for a moment and think about ourselves—not in terms of who we are or what we like or dislike, but rather the sheer numerical complexity of each of us. Contemplate our unique genome’s influence in maintaining health and generating disease. Consider our incredible complexity—and please excuse us if our math is not precise. We did double-check!
Humans:
- make red blood cells at an astounding, incomprehensible rate of about 2 million per second.
- are composed of 30 to 40 trillion cells, with RBCs being the largest single-cell type yet accounting for less than 5% of our total mass. The bacterial count within and on our bodies likely outnumbers our somatic cells.
- have smooth blood conduits throughout; if laid end-to-end, would circumnavigate the Earth over two times, about 60,000 miles.
- have abundant DNA that taxes our ability to fathom the size and length of this component. Each body cell contains about 2 meters of DNA. Assuming the lower estimate of 30 trillion cells, we have enough end-to-end DNA to go around the Earth 1.5 million times. Stated another way, it’s enough to go from the Earth to the Sun (93 million miles) almost 400 times. DNA is about 6 microns in diameter and is not an unmanageable tangle despite the tight quarters. It is packaged in a manner that permits ready access to the many enzymes in the cell that use it to do their work, namely encode proteins, do repairs, and even replicate.
A cautionary tale of the technology: Jesse Gelsinger
Jesse was one of the first patients to undergo gene editing to treat a rare metabolic disorder causing lethal ammonia levels to accumulate. Over half with the condition die within a year of birth. As a 17-year-old, Jesse’s condition was managed with a restrictive diet and four dozen pills each day.
Jesse enrolled in a trial at the University of Pennsylvania, where he underwent gene editing, and within a day, he experienced jaundice, intense systems-wide inflammation, and multiorgan failure; he died three days later. The news rocked the medical world, dealing a particularly severe blow to the gene editing community. Jennifer Doudna (a co-recipient of the Nobel Prize for CRISPR/Cas9), whose work was not involved, said, “Jesse’s death made the whole field of gene therapy go away, mostly, for at least a decade.”
Important questions to consider
Gene editing should prompt us to ask the tough questions. New healthcare interventions should be approached cautiously and conservatively, as the downstream consequences may not always be fully appreciated.
Relevant to gene editing:
- Could an inflammatory response be triggered by the virus used?
- Is there any chance the deactivated virus might reactivate, potentially causing disease?
- If a gene is inserted incorrectly, might it lead to cancer or some other unanticipated serious side effect?
- Should the process be utilized if it is too expensive, laborious, or insufficiently efficacious compared to traditional interventions?
- What are the ethics of manipulating DNA? If we can edit bad genes, can we not introduce designer genes to create ‘superhumans’? What about creating docile humans who mindlessly do what they are told to do?
- What might the outcomes be of the potential marriage of artificial intelligence with gene editing? Should we embrace this, or should we be wary.
The new generation of gene therapy is likely much safer than it was 25 years ago, with important and sobering lessons learned since Jesse’s 1999 death. But just how safe is it? Do the benefits sufficiently outweigh the risks in the era of personalized anesthesia? Do we even have the tools and knowledge to gauge the risk adequately?
Gene therapy in personalized anesthesia—really?
Advances in our understanding of genetics greatly impact the decisions that CRNAs make. This is the domain of pharmacogenomics and precision medicine. Knowledge of genetic variation in receptors and the activity of hepatic and blood enzymes reveals the reasons for many of the variable drug responses we see throughout the perioperative period.
Consider succinylcholine and how mutations in butyrylcholinesterase (pseudocholinesterase) encoders affect its activity. Ponder how mutations in the gene that metabolizes codeine necessitated an FDA Box Warning due to deaths in children. Then, reflect on the pharmacogenetic disorder, malignant hyperthermia (MH), and its patient safety implications. Appreciating the genetic fundamentals of a disorder is the start of a pathway to its genetic repair.
Research and clinical work on postop cancer recurrence are robust, and one investigator whose work we’ve followed at the University of California San Francisco envisions gene therapy playing a significant role that is, at this time, still largely theoretical. Other work worldwide involves treating acute and chronic pain, particularly neuropathic pain.
Given the opioid epidemic and the current limitations of good analgesic options for chronic pain, newer experimental agents will continue to emerge. By targeting a specific receptor or another molecular target, gene therapy may provide excellent analgesic efficacy for pain treatment without the side effects seen with current pharmacotherapies. This may be a particularly fertile domain for clinical application.
Consider just one application: phantom limb pain. Imagine a patient scheduled for limb amputation who, in the days or weeks before the procedure, undergoes gene editing to produce long-term postoperative analgesia. On the day of surgery, you employ a regional or general technique and a multimodal approach for perioperative analgesia. The patient is comfortable with short and long-term follow-up, revealing no need for opioids and no symptoms associated with the phantom limb syndrome. Is this even possible? Yes, this is likely to happen.
Here is a short list of potential targets of gene therapy in anesthesiology: increasing myocardial tolerance to ischemia, preventing acute kidney injury, extinguishing a drug allergy, eliminating nausea and vomiting, and transforming a patient at risk for MH into one who is not. Science fiction? Not from what we see happening in the growing literature on genome editing.
Where we are today
The clinical applications of genetically editing specific molecular and biochemical targets are slowly but inexorably moving to the patient’s bedside. Given the ample clinical need, chronic pain represents a domain sorely in need of additional therapies and may be the first syndrome to emerge with FDA-approved tools for anesthesiology.
Even if the merits of direct clinical application of gene editing seem remote, consider this: basic science research has a long and robust history of creating pathways and opening doors to applications previously not even considered. Stay tuned; you may be surprised at what lies beyond the horizon, but what may soon come into view.
Ketamine has experienced a renaissance from the drug’s initial use many years ago. Not only as part of a multimodal component of many anesthetic approaches to reduce opioid use but more recently as a drug to manage emotional and psychiatric issues. As nurse anesthetists, we have a responsibility to understand where we are with ketamine, especially as we consider its use in ambulatory “ketamine clinics.”
Table of Contents
- Ketamine and the fruit fly
- The remarkable clinical resurgence involving ketamine
- Clinical considerations
- Clinics are proliferating
- S-ketamine (marketed as Spravato®)
- Psilocybin—the magic mushroom
- Where are we with ketamine?
In October 2023, the popular “Friends” actor Matthew Perry, who acknowledged drug and alcohol problems for many years, was found dead at his Los Angeles home. The attending coroner cited his death as multifactorial but primarily due to “the acute effects of ketamine.” Perry was undergoing ketamine infusion therapy, but his autopsy revealed the fatal episode was not related to his most recent therapy session, which occurred 10 days before his death. Perry’s death aroused and focused widespread public attention on ketamine infusion clinics as well as microdosing of other CNS-targeting agents like psilocybin.
What is the clinical status of ketamine and other CNS-altering compounds like psilocybin for treating mental health issues? And what do we know about the many CRNA-managed, free-standing ketamine clinics that have emerged nationwide?
Ketamine and the fruit fly
You should not be surprised that the lowly fruit fly, Drosophila melanogaster, has taught us a thing or two about how ketamine works, given the remarkable legacy of the fly in genetic and pharmaceutical research. What’s known is that many of the drugs currently used to treat depression and anxiety act by altering CNS serotonin levels. Fruit flies conveniently use serotonin as a central transmitter, providing us with a surprisingly valid model to study its effect on the brain. There is even a mutation, dSERT (Drosophila serotonin transporter), that researchers used and just published in the highly regarded Journal of Neurochemistry, demonstrating that microdosing ketamine does not block serotonin reuptake but rather causes complex behavioral changes mediated by glutamate and serotonin receptors.
Now, that might not seem like a huge deal to the uninitiated. Still, it reveals what is being seen clinically by providers and patients alike—that ketamine, and likely other compounds, may work to alleviate depression by mechanisms previously unattainable by our existing pharmacopeia.
Similarly, recent work demonstrates that ketamine, an N-methyl-D-aspartate (NMDA) receptor antagonist, may revolutionize the treatment of depression because of its potent, rapid-onsetting, and sustained effects to relieve depressive manifestations. Of course, this has created a bit of a conundrum as the elimination half-life is briefer than its effect in relieving depression. There is still a lot to learn about how ketamine works to alleviate mental health issues–which we have a responsibility to do.
The remarkable clinical resurgence involving ketamine
For CRNAs who have been in practice for over 20 years, the movement to use ketamine to treat depression, PTSD, and even bipolar conditions in free-standing clinics owned and operated by CRNAs likely comes as a remarkable renaissance. Synthesized as CI-581 in 1962, it was widely used as a veterinary anesthetic. Its analgesic potency, preservation of sympathetic tone and airway reflexes, and its unique dynamics in creating a dissociative anesthetic state led to human use, marred by its tendency to cause emergence delirium and other unpleasant states of mind. With few exceptions, ketamine departed from routine clinical practice until it was resurrected as part of a multimodal, opioid-sparing analgesic technique, which coincided with incidental observations that it could sometimes remedy depression.

Clinical considerations
Many CRNA clinical entrepreneurs have subspecialized in the treatment of depression and related conditions using therapeutic microdosing of ketamine in free-standing clinics. The impetus came from U.S. studies, favorable case reports, and international publications. This body of animal and human research demonstrates that ketamine is often effective in treating major depression, bipolar disorder, and acute suicidal ideation. The careful titration and only moderate degrees of receptor occupancy can be advantageous to achieve its depression-relieving effect and avoid dissociative and psychomimetic activity.
In an August Up-to-Date, the authors noted that randomized trials of IV ketamine for treatment-resistant depression have traditionally occurred in academic settings with collaboration among expert providers. However, they acknowledge that freestanding ketamine clinics are now common, with treatments dispensed by providers who often have limited to no experience in treating depression, which they consider concerning. They also note that many patients are now treated with oral ketamine taken while at home and without a certified provider present.
The Up-to-Date authors note that ketamine is an NMDA receptor antagonist but emphasize that it is not clear whether this produces its antidepressant effects. Trials revealing that racemic ketamine was not as effective as its stereoisomer, S-ketamine, illustrate this point. Clinical and bench research suggests that ketamine may activate other brain components or increase connectivity among brain components.
Ketamine’s optimal delivery method has not been established. While most of the published work—and apparent use in free-standing clinics—involves IV administration, it can also be given intramuscularly, intranasally, orally, subcutaneously, or sublingually. Dosing and administration methods vary considerably among the providers offering the service.
We logged onto several CRNA-managed sites and learned about their services. There are even ketamine infusion clinic courses available for purchase; two that we visited, each offered by a CRNA, are a one-stop shop for what you need to know. They introduce what constitutes a clinic, how to set one up, what the indications are, how to administer the drug and the evidence for the treatment. Dosing strategies vary considerably, as noted in the Up-to-Date article, as there is considerable debate about what constitutes the best-evidence approach for a given patient.
One of the websites we visited has a chatline person ready to answer any questions (we did not ask any) and has in bold lettering, “Becoming a ketamine therapy provider will allow you to earn a high income, reclaim your schedule, and help patients.” A testimonial by one CRNA clinic owner/manager reported that his previously exhausting clinical schedule in his OR job was now rewarded by a practice that provided him with a better work-life balance.
The AANA maintains a website dedicated to ketamine infusion clinics and offers relevant information and guidance for the interested. One of the many areas covered includes responses to a multi-question survey of CRNAs who provide infusion services. Regarding the question of: “What is the patient’s diagnosis being treated with ketamine infusion therapy,” these were the responses:
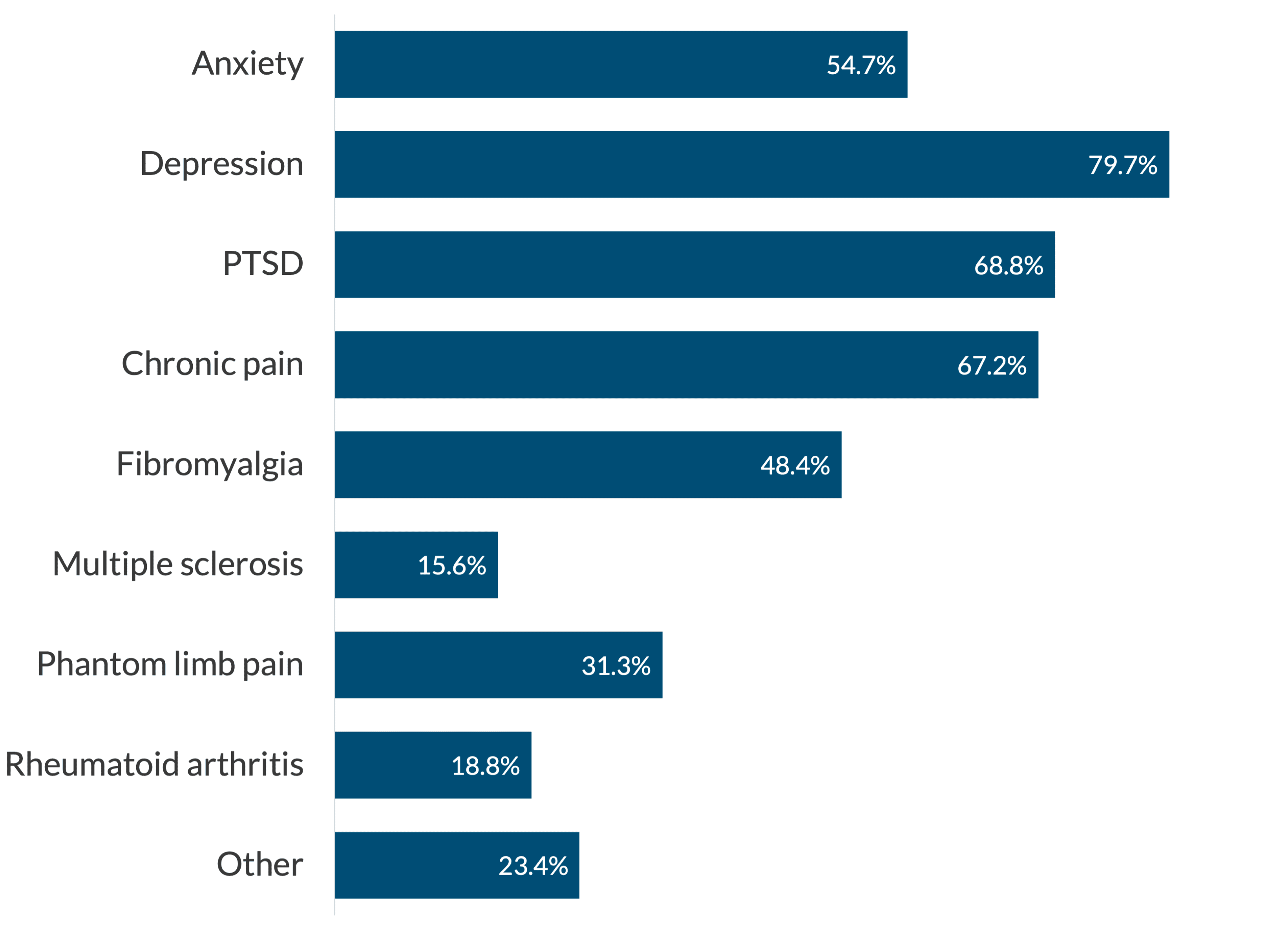
The “other” diagnosis included TMJ syndrome, cancer pain, migraine headaches, new onset daily headaches, post-Lyme disease, neuropathic disease, obsessive-compulsive disorder, gambling addiction, postpartum depression, bipolar disease, and high opioid use. A remarkably diverse group of conditions!
Clinics are proliferating
Our research found that the role of the CRNA, or other “elite nurse practitioners,” as one website refers to the providers, is defined by each state’s Board of Nursing Scope of Practice, which varies regionally. It is impressive that the number of clinics continues to increase, apparently in response to an escalating demand for their services.
With the number of clinics skyrocketing, there are cautions by authoritative figures concerned that it is an unregulated industry with the potential for misuse and patient safety issues. Ketamine is an FDA-approved drug that is increasingly prescribed off-label. There are concerns that its use in this domain may be jumping ahead of the evidence, with patients receiving treatments that have not been well-studied, validated, or guided by multidisciplinary consensus committees. Smita Das, MD, PhD, is one of many mental health experts we encountered who raised concerns. Dr. Das, a Professor of Psychiatry at Stanford University, chairs the American Psychiatric Association’s Council on Addiction Psychiatry and is vocal in urging caution. Consider too, that the treatments can be expensive, up to $1,000.00 per session, and are generally not covered by insurance.
S-ketamine (marketed as Spravato®)
S-ketamine, or esketamine, is an enantiomer of ketamine hydrochloride. Think of it this way: an enantiomer is one of a pair of non-superimposable molecules, mirror images of each other. A good illustration of this is by looking at your hands. While they are essentially mirror images of one another, they cannot be superimposed.
Esketamine has greater potency than ketamine. It is not used as an infusion but as a nasal spray under direct medical supervision. The FDA issued a boxed warning (its highest safety warning) for Spravato® because of potentially serious adverse events, including significant anesthetic effects, respiratory depression, and extremely high abuse potential. It appears to be available only through a special restricted distribution system, the FDA’s Risk Evaluation and Mitigation Strategy. It is only administered in certified medical offices where specified monitoring strategies are used.
Esketamine is used far less frequently than the traditionally marketed ketamine hydrochloride. The free-standing ketamine clinics appear to be taking a more conservative approach to treating depression on an ambulatory basis until more evidence emerges about the safety and dosing of esketamine.
Psilocybin—the magic mushroom
Psilocybin is a tryptamine derivative that enhances CNS serotonin levels and is now approved for select clinical trials for treating treatment-resistant depression, post-traumatic stress disorder (PTSD), and suicidal ideation. Psilocybin comes from the Psilocybe and Panaeolus species of what are commonly called “magic mushrooms.” The four-part Netflix series, “How to Change Your Mind,’ based on the journalist Michael Pollan’s book, ignited a lot of public attention on microdosing to treat depression and enhance conscious experiences.
The saga of psilocybin is a rapidly evolving story, what some refer to as “the psychedelic renaissance.” The growing experience with psilocybin adds to an ever-enlarging pool of clinical and patient safety data relevant to treating mental health. Legal guidelines and frameworks are currently being revised for this Schedule I compound. Some cities (like Oakland, CA, and Washington, DC) soften their criminalization, while other locales (like California and Oregon) provide state-wide legalization.
The National Drug Intelligence website has this posted: “Psilocybin is illegal. Psilocybin is a Schedule I substance under the Controlled Substances Act. Schedule I drugs, which include heroin and LSD, have a high potential for abuse and serve no legitimate medical purpose in the United States.” Some states and cities have enacted legislation challenging this stance.
Psilocybin has hallucinogenic effects and is available in natural and synthetic forms. There is a growing interest in its use in treating addiction, depression, anxiety, alcohol abuse, PTSD, and several emotional and psychological conditions. Its legal status and guidance regarding its use to treat emotional and physical infirmities is very fluid.
A brief note about MDMA
Lykos Therapeutics spent a great deal of effort, and money, to seek FDA approval of MDMA (3,4-methylenedioxymethamphetamine), also called “Molly” or “Ecstasy,” for treatment of PTSD. On August 9, 2024, approval was denied by the FDA for this synthetic drug that has effects similar to stimulants such as amphetamine-like compounds. If MDMA had been approved, it would have been the first new therapeutic drug for PTSD in a long while and would have given Lykos full control of the agent for 5 years.
There were a number of issues that surfaced including faulty studies of its effectiveness and safety concerns. For now we will leave it at that, but rest assured we will be keeping this on our radar as further developments in the area emerge. Given Lykos’ interest in the agent, we suspect there is more to come!
Where are we with ketamine?
Although the marketplace is in flux, the latest administrative data suggests that as many as 750 ketamine clinics nationwide generate revenues well north of 3 billion dollars annually. The number of for-profit clinics will likely continue to increase given the wide range of identified conditions that some suggest the drug can treat. Revenue generation is projected to double within 5 years. This is somewhat concerning, given that the insurance industry has largely shown disinterest in covering the service.
The FDA has not approved ketamine for use in any mental health treatment, resulting in providers formulating their treatment strategies and interventions for off-label interventions. Esketamine is FDA-approved for “breakthrough therapy” when administered under close medical supervision. Given the variability among providers in how they use ketamine to treat an expanding range of conditions, we will likely see lots of activity in professional and lay literature as well as in social media. Equally likely is the attention it will catalyze in legislative and regulatory proceedings.
As CRNAs ourselves, we understand the challenge of fitting CRNA continuing education credits into your busy schedule. When you’re ready, we’re here to help.