Cricoid pressure was first described in the 1770s to prevent stomach insufflation during artificial ventilation of the lungs. However, it was not until 1961 that Sellick promoted cricoid pressure (Sellick maneuver) to prevent regurgitation and aspiration with the induction of anesthesia in the obstetrical population. He described the “temporary occlusion” of the upper esophagus by applying a backward force upon the cricoid ring to prevent stomach contents from reaching the pharynx.
The cricoid cartilage is located and palpated between the thumb and second finger, and the index finger applies moderate pressure with induction of anesthesia before the loss of consciousness. As consciousness is lost, firm pressure is applied without obstructing the patient’s airway. In Sellick’s description, the patient was placed with the head and neck fully extended (tonsillectomy position) and the “head down slightly with the head turned.” Patients today aren’t positioned in a head-down position for a rapid sequence induction. Since Sellick’s original description, the application of cricoid pressure has become an unofficial component of a rapid sequence induction of anesthesia in patients with a “full stomach,” and when omitted, may be cited by the legal profession as evidence of substandard care.
| Table of Contents
- What’s the Evidence?
- Cricoid Pressure and the Pediatric Patient
- Is Aspiration Troubling in the Pediatric Patient?
- Application of Cricoid Pressure in Pediatrics
- Where Does This Leave Us?
Effectiveness and risks of cricoid pressure during intubation
Cochrane database review published in 2015 only found a single publication (from 493 evaluated) that contained all the essential criteria of a randomized control trial. This review did not examine the efficacy of cricoid pressure, and the authors concluded that there are no available random controlled trials examining outcomes following the application of cricoid pressure during rapid sequence induction.
Cricoid pressure and the pediatric patient
Appropriated from its application in adults, the effectiveness of cricoid pressure in the young child remains empirically derived, limited, and absent scientific appraisal.
Salem studied the application of cricoid pressure in eight-fresh infant cadavers finding that cricoid pressure was effective in sealing the esophagus against intra-esophageal pressures up to 100 mmHg.
Edington reviewed the use of cricoid pressure in a teaching hospital, finding its application varied between 5-34% among nine anesthesia providers. A survey of pediatric anesthesia providers in 1994 found that only 50% of the anesthetists applied cricoid pressure when anesthetizing infants for pyloromyotomy.
A similar survey published in 2001 found that clinicians only utilized cricoid pressure in 40-50% of children who were thought to benefit from its application. In a reported survey of pediatric anesthesiologists, 90% reported employing cricoid pressure, but only 68% believed that cricoid pressure prevents passive regurgitation.
Is aspiration troubling in the pediatric patient?
Warner and colleagues prospectively identified all cases of pulmonary aspiration over two years during the perioperative period in 56,138 consecutive patients under the age of 18 years. Children who underwent anesthesia for emergency procedures had an increased risk of aspiration (1:373 versus 1:4,544). Children under three years of age who aspirated had a preoperative bowel obstruction or ileus. Three of these children required mechanical ventilation for more than 48 hours. There were no deaths due to pulmonary aspiration. This study found that the pulmonary aspiration of gastric contents and serious respiratory complications in healthy children under 18 years of age are uncommon.
Application of cricoid pressure in pediatrics
Differences between the adult and the pediatric cricoid cartilage include the size and a higher position in the pediatric patient (C3 – C4 interspace versus the adult position of C5 by age 6). Identifying the cricoid cartilage in children using surface landmarks is frequently incorrect and frustratingly difficult. In an observational study of 30 pediatric patients aged 0-6 years, “in all but one patient, there was a measurable difference found between where the cricoid was thought to be and where it was actually visualized by ultrasound.” Correctly identifying the cricoid cartilage is essential if cricoid pressure is considered a crucial protective strategy in the pediatric patient.
The incorrect application of cricoid pressure may:
- Distort airway anatomy with misalignment of the larynx and trachea.
- Interfere with the position of the laryngoscope blade.
- Produce hypopharyngeal compression.
- Inhibit ventilation and placement of a supraglottic airway.
- Stimulate upper airway reflexes resulting in coughing, hiccoughs, and vomiting in the lightly anesthetized.
The efficacy of cricoid pressure in preventing the aspiration of gastric contents is dependent upon the anatomic relationship of the cricoid to the esophagus. The anatomical relationships of the pediatric airway mimic those of the adult by age 8. In a retrospective study of children aged 0-17 years who had cervical spine or neck CT scans, Dotson and colleagues found that a third of the children had left lateral displacement of the esophagus from the cricoid. They also found the esophagus laterally displaced in nearly 50% of children under eight. If the application of cricoid pressure produces further lateral displacement, it would seem logical esophagus occlusion would not occur.
How to apply cricoid pressure
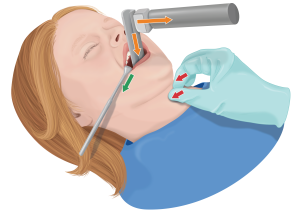
The application of cricoid pressure may lead to resistance and struggling, increasing intraabdominal pressure, and precipitate vomiting. In the single-handed technique, the thumb and middle finger are placed on either side of the cricoid to prevent lateral displacement. The index finger applies pressure directly upon the cricoid. The individual applying cricoid pressure stands on the patient’s side according to the applicator’s dominant hand. For example, when applying cricoid pressure with the right hand, the applicator is positioned on the patient’s right side, resting the palm upon the sternum to avoid interference with the insertion and manipulation of the laryngoscope. The free hand may be placed under the neck and occiput to maintain the desired intubation position. The illustration shows the various force vectors needed for a successful pediatric intubation with cricoid pressure.
Walker evaluated the force required to occlude the subglottic airway by 50% in children during bronchoscopy with the application of cricoid pressure by a force monitor. The overall force required to compress the airway by 50% was 10.5 N, but as low as 5 N in children under one year. Teenagers required a pressure between 15 and 25 N to compress the airway by 50%. The currently recommended force in the adult is 30 N (3 kg of force), which would be excessive in all pediatric patients.
It is essential to preoperatively identify the pediatric patient at risk for aspiration: children with abdominal distension, bowel obstruction or ileus, post-tonsillectomy bleeding, or those who have recently consumed a meal. Then, the most experienced individual should apply cricoid pressure to the pediatric patient.
Final thoughts on the cricoid pressure maneuver on pediatric patients
There will likely never be, a randomized controlled trial of the efficacy of cricoid pressure in pediatric patients with a full stomach. Although scientific evaluation of the effectiveness and safety of traditional techniques applied to patients at risk for aspiration during anesthetic induction and airway management is desirable, use cricoid pressure, knowing it is not failsafe.
While supported by various cadaver and animal studies, cricoid pressure is but one component in a broad umbrella of interventions designed to minimize the overall risk of aspiration of gastric contents. And finally, like any other intervention, the efficacy of cricoid pressure is operator-dependent. Education, training, practice, and evaluation of the application of cricoid pressure in pediatric patients are essential.
Your action plan
- Reflect on your last pediatric patient at risk for aspiration. Knowing what you know now, what (if anything) would you have done differently?
Want to earn Class A credits while staying up to date on current anesthesia practice? Check out our CPC Core Modules and CRNA Updates courses.







