| Table of Contents
- Introduction
- The Case for Color-Coding Drug Syringe Labels
- The Case Against Color-Coding Drug Syringes
- Uniqueness of the Anesthesia Workstation
- Where Does this Leave Us?
______________________________________________________________________________________________________________
Helping or hurting: color-coded medication labels for syringes
The Institute of Medicine (IOM) reported that more than 1.5 million Americans are injured annually in our hospitals, with medication error a common responsible mechanism. Although rates differ widely among settings, the IOM suggests that patients can expect an average of one or more potential medication errors daily during their hospital stay. Many different initiatives to mitigate their occurrence are used.
Remarkably, our literature search did not find the phrase “medication error” used until 1966 and still much later involving surgical anesthesia. One contentious intervention relevant to medication error mitigation that impacts the CRNA is color-coded labels (CCLs) for syringes. CCLs generate strong opinions in two broad camps.
Okay, let’s say it and own it: human variability and its associated error pose a significant risk for our patients. In everyday practice, CRNAs use what are classified as high-alert medications (HAMs). Many of these are arguably some of the most dangerous agents on Earth that are intentionally administered to a patient. For example, consider this incomplete list of HAMs that we use:
- Opioids
- Paralytics
- Potent inhaled agents
- Anesthesia induction agents
- Anxiolytics
- Adrenergic agonists
- Adrenergic antagonists
- Antiarrhythmics
- Anticoagulants
- Potassium containing solutions
- Insulin
- Neuraxial and peripheral local anesthetics
Complicating the matter significantly are concerns with the “look-alike” packaging of medications and different concentrations of the drugs in various formulations of the same agent. For example, heparin comes in at least 5 different concentrations in the U.S. Exparel, propofol, and clevidipine, are all milky white lookalikes. Blue vials of hydralazine and phenylephrine are nearly identical. The small vials of midazolam and dexamethasone are uncannily alike in their packaging.
Compounding the issue for CRNAs is production pressure, stress, multitasking, and that we retrieve the drug from a cart, draw it up, label it, and administer it—as soloists. The thinking that initiated the CCLs involved standardizing the doses and having the drug in a ready-to-use form. Let’s take an open-minded look at CCLs.
The case for color-coding drug syringe labels
OK, CCLs may not be perfect, but let’s not prematurely discard something that may have merit. Instead, think of the “Swiss Cheese” model of error genesis, describing how several small failures may align to create a pathway for an error to impact a patient and cause harm.
A few ways that we create layers of safety to avoid alignment include:
- Backup laryngoscope in case of bulb failure
- Preventing hypoxic gas administration (Pin index, alarms, proportionator, etc.)
- AMBU or another secondary source of ventilation
- Backup source of O2 (E-cylinder)
- Backup airway management device (Glidescope, bougie, LMA, etc.)
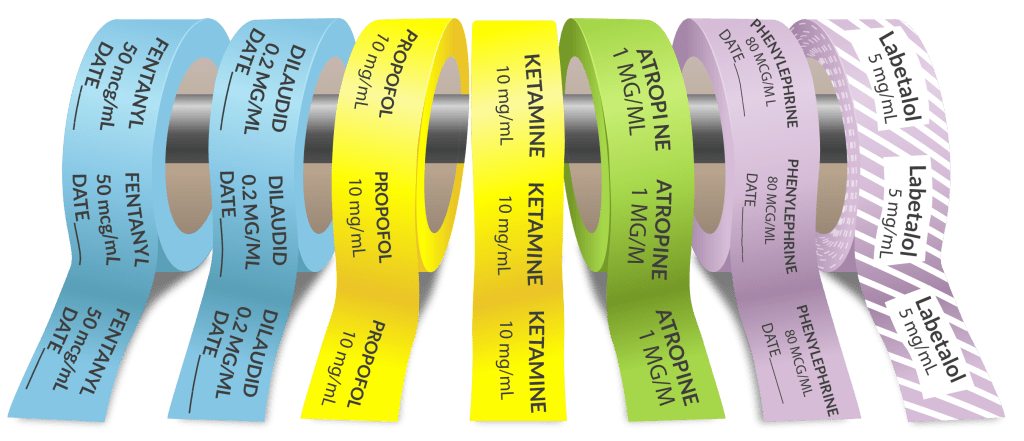
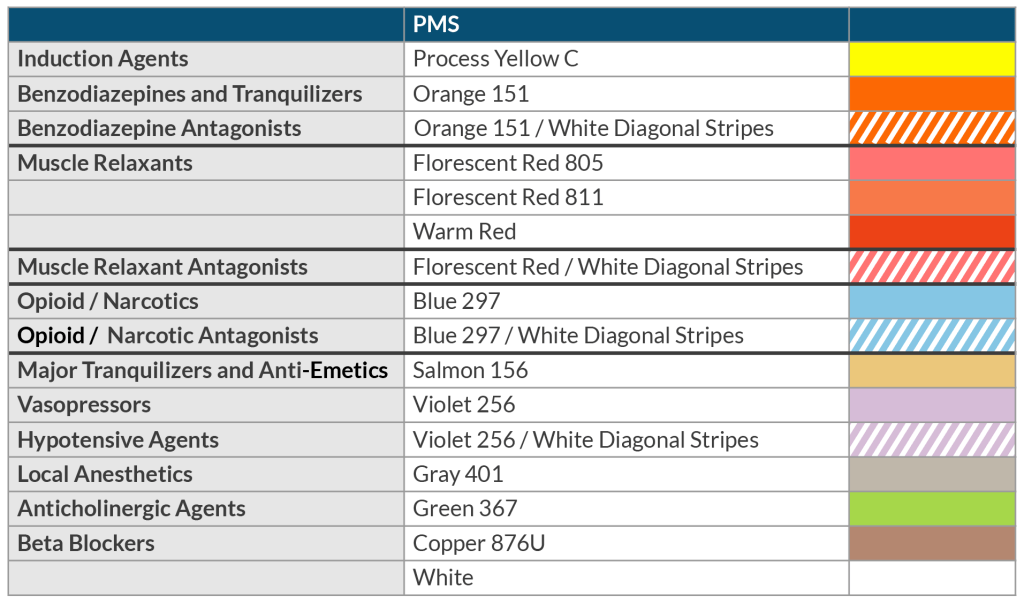
Perhaps we should consider CCLs as just another “cheese layer” to prevent an error from reaching the patient. Going back to 2015, the ASA went on record supporting the application of CCLs to our syringes, available in 9 unique pigments, each specific to a drug class. A good deal of psychological and engineering research identifies color as essential in discerning what is in our world. Such research led to using standard colors in road signs, traffic lights, electrical wiring, national flags, the aviation industry, and even in the culinary world. The latter refers to different color cutting boards that chefs use to mitigate the risk of allergy, such as a red board for meat, a white one for dairy, a green one for fruits and vegetables, etc. Humans are hard-wired to identify things in color!
Human factors to consider when labeling medication
Designing something to help us do the right thing is the goal of human factors engineering. The burner controls on your stove, a light switch, a cell phone touch screen, and even a doorknob is engineered to help us get it right. The fundamental basis for human factors engineering is presuming that humans will fail and make the task at hand minimally reliant on recall, performing a calculation, and hypervigilance.
The fundamental premises of color coded labels fall into 2 categories. First, they function as an additional component of identifying something: lettering plus colorization. Put another way, CCLs serve to lower the risk of misidentification. Second, CCLs are designed to reduce syringe swaps and dosing errors, which account for most anesthesia drug errors.
The mandates of drug administration: the 7 “rights” plus 3 we are tacking on
It’s easy to become complacent when administering an IV drug for various reasons. But when you think about it, we give a drug straight to the heart, brain, liver, kidneys, etc. Yikes!! It’s very sobering when you think about it! Our early nursing education taught us the 7 “rights” of giving a drug. These were the right patient, -drug, -dose, -time, -route, -reason, and -documentation. Under the “right drug,” labeling is critical, so let’s add 3 subscripts:
- Read the label carefully when retrieving the drug
- Reread it when preparing and labeling the syringe
- Read it once again before discarding the ampule.
It’s just a piece of the puzzle regarding pharmaceutical labels.
Drug errors are not just due to syringe swaps. There are errors in drawing up the drug and in preparing its administration. We may select the incorrect vial (especially common with look-alikes), give the wrong dose, or administer it to the wrong patient. On top of it all, communication errors are common. We hold patients’ lives in our hands and must do all we can to minimize error. CCLs and mindful reading of the label in tandem can go a long way in mitigating drug error.

The case against color-coding drug syringes
Looking at misadventures in and out of our specialty can be very illuminating. Brace yourself as we describe two cases from the Institute for Safe Medical Practice (ISMP) website. A 20-year-old gave premature birth via C-section one day before she died from swine flu. The infant was fed via an N/G tube. One week later, the infant died minutes after a nurse, using a correctly lettered CCL syringe, injected feeding formula IV instead of via the N/G tube. In another case involving an adult, a nurse using a CCL syringe administered liquified yogurt IV instead of the N/G tube. The patient succumbed. The Anesthesia Patient Safety Foundation’s Pro/Con debate on color-coded medication labels echoes similar concerns, warning that color-coding can foster complacency and reduce vigilance when reading syringe labels. The ISMP does not endorse CCLs, viewing them as fostering complacency and not carefully reading the label.
Over reliance on color can impede reading
Consider this report found in the database of the Anesthesia Quality Institute describing unfortunate events at one of the nation’s premier pediatric institutions, The Children’s Hospital of Philadelphia, with its competent staff of anesthesia providers. Prefilled anesthesia drug syringes prepared by an automated robot are affixed with printed black letters on white labels. Here it appears the providers were overly reliant on color-coding instead of reading the label.
As reported, the hospital pharmacy began making prefilled hydromorphone syringes with white labels when their out-of-hospital vendor, who supplied the drug with light blue labels, couldn’t meet the demand. As a result, anesthesia providers, long accustomed to seeing dexmedetomidine with white labels, incorrectly administered the wrong drug to 3 patients. Each case involved identifying the syringe’s content by label color rather than lettering. Did habit, rote memory, and complacency contribute?
Difficulty discerning similar colors
We should also consider the challenge to a color-blind provider and the limited number of available colors that can be easily differentiated from one another. The psychology of choosing something from a large group of choices, whether it’s shoes, clothing, breakfast cereal, what to watch on Netflix, or of more significant implications, a syringe with a CCL, can lead to confusion and undermine safe practice. Over-reliance on a CCL ignores the three additional steps we added to the “7 rights.”
The uniqueness of the anesthesia workstation
As noted earlier, the CRNA is a solo retriever, preparer, labeler, and dispenser of the drugs they administer. But beyond this is the potential to contaminate the drugs we prepare as the task is performed in an unsterile environment that does not comply with the guidance outlined in USP 797, preparation of sterile medications.
Final thoughts on the debate of color-coded medication labels

We’ve outlined some of the pros and cons of CCLs. The OR and the anesthesia workstation are not static, but rather in continuous evolution. While technology drives much of that evolution, it must coexist with the more consequential goal of ensuring patient safety.
To this end, the safe medication practice movement will likely include a growing emphasis on prefilling and pre-labeling drugs before arriving at the OR. Prefilling and pre-labeling are performed by an in-house pharmacy (likely one dedicated to the OR) or by an outsourced medication distributor. In either case, CRNAs will likely encounter CCLs of drugs by category (e.g., opioids, sedatives/hypnotics, antibiotics, paralytics, etc.). We also want to encourage a CCL add-on, barcoding! As we find ourselves increasingly removed from drug preparation, variations in drug concentration are likely to be encountered, so additional safety features are welcome.
Consider your view of the CCLs, and how it intersects with medication safety. CRNAs are experts in selecting, administering, and monitoring the effects of potent and dangerous drugs. It’s what we do. Getting it right takes us back to those 7 rights and the 3 subscripts we added here. We like the relevance of that NikeTM slogan, “Just do it!”
As CRNAs ourselves, we understand the challenge of fitting CRNA continuing education credits into your busy schedule. When you’re ready, we’re here to help.






